The main surgical options for treatment of urge related incontinence include:
Intradetrusor botulinum toxin injection
This treatment, performed under a local anaesthetic with a flexible cystoscopy, works very well for patients with neuropathic overactive bladder (eg multiple sclerosis patients who are catheter-dependent who leak with bladder spasms) and also for those with unknown (idiopathic) causes for their overactive bladder It’s efficacy is in the region of 70% but problems include urinary retention (around 15% will need to have a urinary catheter or perform clean intermittent self catheterisation) and the need for repeat injections (on average every nine months). To date, no significant problems have been encountered after multiple repeat injections. There has also been no reported loss in efficacy and no ultrastructural changes in the bladder with repeated injections.
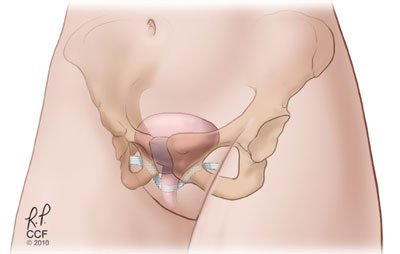
Sacral neuromodulation
Sacral nerve stimulation (SNS) is a continuous use of mild electrical impulses delivered through an implanted device mainly to S3 nerve root in the sacrum. The exact mechanism of action is not known but is thought to modulate the local neuronal reflexes and inhibit bladder contractions. (SNS) is delivered through an implanted device in the lower back with the lead positioned near S3 nerve root.
This is a minimally invasive procedure and can be performed under local or general anaesthesia. It is generally performed as a 2-stage procedure.
The first stage is known as percutaneous nerve evaluation. It is required to assess whether neuromodulation will be effective for a given patient. The surgeon uses a small needle to place a thin wire in contact with S3 nerve root. The other end of the wire is taped to the back and connected to a temporary stimulator control unit, which is worn on the belt. This is worn for one to three weeks to assess the response. The response rate is between 60 to 80%. If the treatment is effective, then the permanent implant is inserted.
The permanent device is implanted in the lower back / buttock area so it cannot be felt. A handheld wireless patient programmer is used to adjust levels of stimulation as prescribed by the surgeon. The stimulation parameters can be adjusted as needed and the programmer can be switched on and off. The battery has an average life of 7 years and requires replacing after this time.
Enterocystoplasty
This is a major undertaking and should only be done for intractable urgency related incontinence where this is having a major impact on the patient’s quality of life. The principle is to bivalve the bladder and patch the defect with a piece of bowel, often a segment of ileum. This leads to an increase in bladder capacity and decrease in bladder contractions. This is the most definitive procedure to control urgency related incontinence but comes at the highest price. The complications include need for self catheterization (30%), mucus production, stone formation, bacteriuria and urinary tract infections, biochemical abnormalities and long term risk of cancer. Hence, these patients require life long follow up with regular blood tests and yearly cystoscopies from 10 years post operatively.
Ileal conduit urinary diversion
This is the most drastic option for control of intractable urgency incontinence. It is a type of non-continent urinary diversion. To create an ileal conduit, the ureters are divided from the bladder and a uretero-ileal anastomosis performed with a 10cm isolated piece of ileum. The other end of the ileum is brought out through a stoma generally in the right iliac fossa. The stoma bag is on continuous drainage and must be periodically emptied of urine, and about once a week, it must be replaced.
Incontinence is a common problem that is often ignored by patients.
There are many simple, successful conservative measures available which can be successfully supplemented by appropriate specialist surgery.
Useful link: Bladder and Bowel foundation (opens in a new tab)