Low back pain
Back pain is very common; eight out of 10 adults will have an episode in their lifetime. It can sometimes come on suddenly and feel very painful but it is very rare that there is a problem that won’t heal and recover with time. Treated with painkillers, remaining active and good advice almost everyone will be improving in a few weeks.
The most important thing to do is to stay active. This prevents the muscles in your back from going into spasm and becoming stiff and more painful. You will need to rest a little too.
Try to stay positive and increase your activity gradually, returning to normal daily activities as soon as you are able. This will prevent your muscles becoming inactive or weaker, and help them continue to support your healthy back joints.
What can cause pain in your back?
Like every joint in your body, the bones in the back are supported by muscles, ligaments, tendons, and other soft tissues such as cartilage. Working together, they provide protection for your spinal cord, and give a strong and flexible central structure. Pain in your back is most often caused by inflammation due to increased stress on one area. This might be one joint of the spine, or it could be one particular structure such as a ligament, tendon or disc. Stresses and strains could be caused by poor posture, holding one position for too long, extreme and sudden movements or repetitive movements. Age related changes (or arthritis) of your back joints can also cause inflammation and be very uncomfortable. All of these should start to feel better in approximately two to six weeks.
What is sciatica?
When we say ‘sciatica’, we mean pain that radiates from the low back, and down the back of one leg along the path of the sciatic nerve. This is far less common than back pain, but is still a very common and painful problem. The likeliest cause of this is the nerve becoming irritated or inflamed in one of the back joints just at the point it exits the spine to travel down the leg, and reporting this back to the brain as leg pain. In some cases, sciatica can be caused by a ‘slipped disc’. This is an old-fashioned term and actually nothing has slipped out of place, so we now call it a herniated disc. Discs provide cushioning between your back bones (vertebrae). The softer centre is protected by a tough and fibrous outer shell. Stresses and strains can cause the soft centre to bulge into the tough layer. This bulge in the wrong place can cause extra pressure or inflammation around the nerve as it exits the spine, possibly leading to pain, tingling, numbness or weakness in the leg.
Age-related changes in the back joints can sometimes have the same effect, reducing the amount of space the nerve has for freedom, and causing some inflammation or pressure. This can lead to the same sensations often referred to as sciatica.

Will my sciatica get better?
Sciatica described above is not an emergency condition and does not need emergency surgery. In virtually all cases the pain in your back and leg get better with time, gentle exercise, and painkillers. This can take longer than simple back pain, but most will be fully resolved in six to 12 weeks. Physiotherapy may help speed up recovery.
Do I need a scan or an x-ray?
Most problems with back pain can be accurately diagnosed with a thorough examination of the back and leg by a doctor or physiotherapist. MRI (magnetic resonance imaging) scans are not required to make a diagnosis, and are not performed in the emergency department for back pain or sciatica. The first line of treatment for back pain or a herniated disc is to allow the back some time to recover. If sciatica symptoms persist for more than six weeks, it is sensible to speak to your GP, a physiotherapist or other healthcare professional for some more specific advice. If your GP or physiotherapist thinks that you may have had a herniated disc and it is not resolving as quickly as it should they may consider referral to the specialist MSK (musculoskeletal) service where further investigations would be considered. Very few patients will go on to have surgery for sciatica that has not resolved on its own.
Cauda equina syndrome (CES)
CES is a very rare but serious condition. It happens because the space for the lowest nerves in the spine has been reduced. This can be caused by a herniated disc, but can also happen with age-related changes in the spine and some other medical conditions. This narrowing causes pressure around the nerves that control the bladder or bowels. These nerves are particularly sensitive so require emergency treatment to ensure they recover.
If you have back pain or sciatica pain accompanied by the following symptoms you must come to the emergency department for immediate assessment:
- Pain in your back which radiates down the back of both legs.
- Weakness or a change in sensation in both legs, or rapidly worsening symptoms.
- New numbness or tingling around your genitals, anus or bottom.
- Sudden or recent change in control of your bladder or bowels.
- Impaired sexual function, such as a loss of sensation during intercourse or new erectile dysfunction.
Finally, please let the doctors know if you have had any of the following as these can all indicate a serious cause: pain at night (eg waking you from sleep), fevers, recent infections, IV drug use, weight loss, or a history of cancer. These are important factors when assessing back pain.
What can I do to help myself and reduce pain?
Your back or leg are likely to be very painful for a few days. Here is what we suggest you do:
- Consider taking painkillers, talk to your local pharmacy about over-the-counter painkillers, or speak to your GP if this does not work.
- Stay active, keep moving.
- Change your position regularly.
- Use heat or ice to relax muscles.
- Use relaxation and positions that are more comfortable to rest sensibly for short periods.
- Try to get plenty of good quality sleep.
- Keep eating healthily; you need good nutrition. Also, stay well hydrated by drinking lots of fluid. Pain medication can cause constipation, which in turn can make you feel quite unwell. Eating and drinking healthily can help prevent this, but speak to a pharmacist about laxatives if you miss a bowel movement.
- Try to return to normal activities as soon as possible.
It hurts when I move, can I make things worse?
Pain is part of our body’s warning system. The threshold is set to make us aware of the potential threat of injury before injury occurs, which helps us to stay safe. It does not follow that the amount of pain is equal to the amount of injured tissue. Slow, gentle movements that you stay in control of are not going to cause injury even in sensitive and healing tissues.
Think about sleeping in positions that keep the body fully supported; use pillows to help support any areas not supported by the mattress. Do stay active, and try to take regular breaks or rests from repetitive activities or activities that keep you in one position for too long, like household jobs or menial data-entry tasks. Change your position regularly, and have a gentle stretch of all the joints in your body. Our spines are designed to move in all directions, so do not avoid particular positions – but be respectful of painful movements. There may be equipment or strategies to make daily jobs easier in the short term, so talking to an occupational therapist may be beneficial.
Regular physical activity will help prevent stiffness and spasm, which can make the pain worse. And, longer term, it prevents the muscles from becoming deconditioned and weak. This reduces the risk of pain or flare-ups in the future.
Back pain exercises
Here are some examples of good exercises to try to start with, and some tips on the best way to do them.
Phase 1
Gentle movements at all the joints in the body will be helpful, general all over body stretches. This will help release your body’s own natural painkiller system.
Use the most comfortable position to gently move and stretch the spine in all directions. This is likely to be lying down on your back or side as all the postural muscles can relax in this position. But it may be sitting or standing.

Lie on your back with knees bent and arms by your side.
Relax your back muscles, tighten your stomach muscles and press the small of your back against the floor, letting your bottom rise, then arch your lower back away from the floor.
Tilt your pelvis forwards and backwards, slowly and gently.
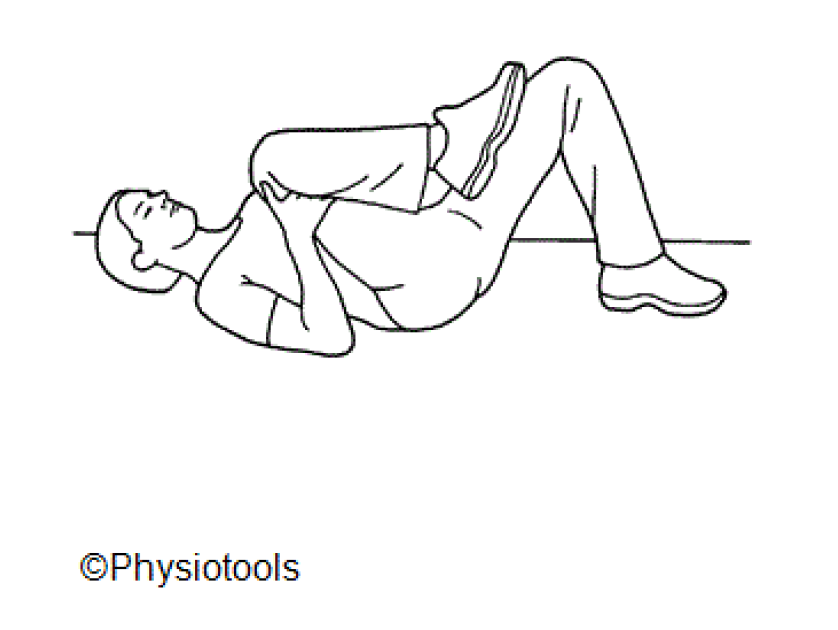
Lie with your knees bent and your feet on the floor.
Lift one knee towards your chest.
Place your hands behind the knee and draw it in to your chest.

Lie on your back with knees bent.
In a controlled manner, move your knees from side to side.
Go only as far as you can without moving your shoulders or letting your back arch.
Phase 2
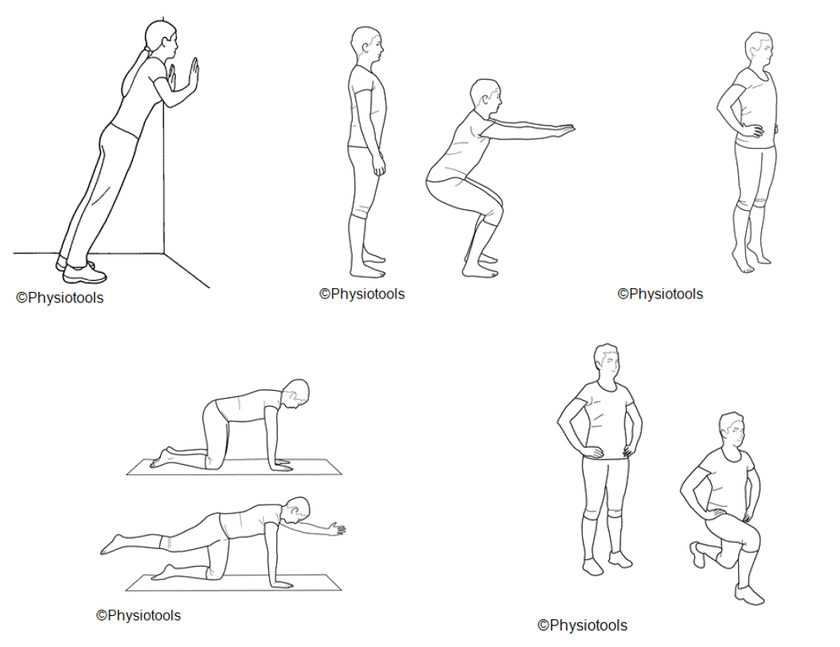
Don’t wait to be 100% better before returning to activity or work. Early movement seems to shorten acute episodes and get them better quicker. Getting back to work as soon as possible has been shown to reduce long term problems. It may be worth talking to your manager about returning to work on light duties or on a phased return. As pain starts to settle, concentrate on exercises that will help prevent further flare-ups.
Think about starting to make yourself stronger and fitter, respecting the pain that may still be settling. You could slowly increase your walking, cycling or swimming in a gradual way. Or you could try strengthening exercise programmes at home. A physiotherapist could help you develop your own personal exercise programme to help prevent future flare-ups. There are also council run exercise referral schemes at your local gym that your GP or physiotherapist could recommend.
Concentrate on exercises that generally strengthen all body parts, but particularly stomach, buttocks, legs and back muscles.

Lie on your back with knees bent.
Draw in your lower abdominal and pelvic floor muscles.
Keep relaxed and breathing maintaining the tension in these muscles but keeping the back relaxed.
Hold for three breaths, and relax.

Bridge
Lie on your back, with knees bent and feet hip-width apart.
Draw in your abdominals and tighten your buttocks.
Tilt your pelvis backwards and lift your pelvis and back up one vertebrae at a time. Lift only as high as you can while maintaining the pelvis position.
Lower your pelvis in a controlled manner.
Find extra information about back pain, and some helpful rehab information here:
- Outpatient physiotherapy (CUH service)
- BackCare - The National Back Pain Association (opens in a new tab)
- Back pain - NHS Conditions (opens in a new tab)
- Back pain - The Chartered Society of Physiotherapy (opens in a new tab)
- Acute back pain - British Association of Spine Surgeons (opens in a new tab)
- Lower Back, Back pain advice and exercises - Dynamic Health (opens in a new tab)
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

