This booklet has been written to provide you, your family and/or carers, with the information you need when using an YpsoPump (without mylife Loop).
Please refer to the additional closed loop supplement if using the YpsoPump with continuous glucose monitoring (CGM) in AutoMode with mylife Loop.
YpsoMed contact details:
- Telephone: Free call UK 0344 856 7820 (24 hours)
- Email: info@ypsomed.co.uk
Please note that the pump companies will not give medical advice and can only offer technical support if you are having problems with the pump.
When using an insulin pump, as part of your diabetes management, it is essential to always have the following items available in case of pump failure and ensure that they remain on your repeat prescription:
- Back-up insulin pens for both quick acting insulin and background insulin (make sure in date)
- Needles for your insulin pens
You will also need a copy of your latest pump settings. These are used to calculate what dose of insulin you need to take if you have to go back to using insulin pens. You will find this information on your latest pump educator clinic letter on MyChart. The pump team can help you work out what doses to take if you are not sure.
In addition, please ensure that you have the following items (in date) at home and on your repeat prescription in case you are unwell, your glucose levels are running high for a period of time or have a severe episode of hypoglycaemia:
- Blood ketone meter
- In date blood ketone strips
- In date glucose test strips
- A copy of the sick day rules
- Diabetes pump team emergency contact details
- Glucagon injection kit (in date – stored in the fridge)
Finally, please check your pump regularly for any cracks or damage and report to your pump company if you have any issues. The company should offer a replacement for broken/damaged pumps if your pump is still within its 4 year warranty period.
Diabetes pump team contact numbers
Please contact the Pump Team if you need advice regarding your diabetes.
For non-urgent queries you can message the Diabetes Educators on MyChart (preferred) or email us on cuh.diabeteseducator@nhs.net (these are checked Monday, Wednesday and Friday). Allow 5 working days for a response. If you require a reply sooner, you can leave a voicemail on one of the numbers below (the answerphone is checked regularly Mon-Fri office hours).
- DSN office: 01223 348790
- Dietitian office: 01223 348769
Urgent advice: Urgent advice
If you are feeling ill or have an emergency diabetes or pump problem out of hours (that cannot wait until the next working day) then contact the Type 1 Emergency Out of Hours number below (or attend your nearest accident and emergency department).
Contact the diabetes educators if you do not have this number.
This is available Mon-Fri 4pm to 11pm and 6am to 9am, weekends and bank holidays 6am to 11pm.
This phone is answered by a diabetes educator oncall. They are not in the hospital and may not have immediate access to your medical notes.
Outside of these hours you are able to call 111 or
Please attend your nearest accident and emergency department for urgent care.
Insulin pump insurance
The insulin pump companies will replace the pump when broken if a technical/mechanical fault is found or through general wear and tear during the 4 years of warranty. However accidental damage or loss due to theft is not covered. You will be expected to personally pay for the replacement of the pump in these cases. Most pumps cost between £2500 and £3000 to replace, so we strongly recommend that you insure your pump under your household insurance or via one of the specialist insulin pump insurance companies.
Support groups and websites
- Diabetes.org (opens in a new tab) - UK charity for people with diabetes
- Funky Jumpers (opens in a new tab) -UK website for clothing/accessories adapted for pump wear
- Hid-in (opens in a new tab) - Accessories for insulin pumps
- Etsy (opens in a new tab) - Accessories for insulin pumps
- Pimp your pump (opens in a new tab) - UK website for clothing/accessories adapted for pump wear
- Insurance 4 insulin pumps (opens in a new tab) - UK site for specialised pump insurance
- Diabetes Technology Network (DTN-UK) | The Association of British Clinical Diabetologists (abcd.care) (opens in a new tab) - UK website with resources and videos
Welcome to your new pump!
The basics of how an insulin pump works
Insulin pump therapy offers the closest insulin delivery system to the way the body would produce insulin without diabetes. An insulin pump uses only quick acting insulin; it delivers it in small pulses continuously throughout the day to meet your background insulin requirements; this is called basal insulin. The insulin pump can then be used to give a bolus of insulin on top of the basal insulin to cover carbohydrate eaten or give a correction for a high glucose reading.
When starting on an insulin pump, your educator will calculate your starting settings. Over a few weeks we will work closely with you to adjust your settings to suit your daily insulin requirements.
Non-urgent advice: Important information
Insulin pumps provide clever technology to better manage glucose levels, but the basics remain important. These include:
- Accurate carbohydrate counting
- Entering all carbohydrates eaten into the pump (except hypo treatment)
- Timing of the mealtime/snack insulin – a bolus given 10-15 minutes before eating is recommended
- Regular set changes
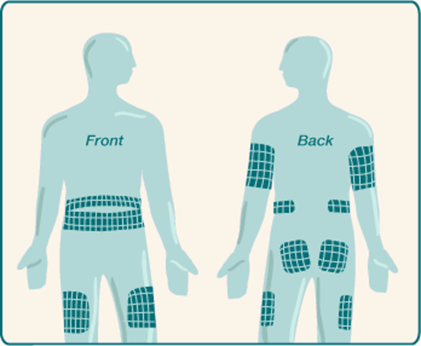
- Rotation of infusion sites
- Optimal hypo treatment
- Adjustments for activity
Reviewing your basal rate
For most people, basal rates vary across the day, and can change with time depending on changes in lifestyle or work. It can take time to work out the right basal rate, but it is important to spend time doing this, as well as checking it every so often, as the amount of insulin that your body needs changes all the time. You may find you need to check if you have a change of job especially if a work day is very different to a non-work day, or if you are going through a particularly stressful period or you have changed your activity levels such as taking up a new exercise regimen.
It is important to ensure your basal rates are correct before you look to make changes to bolus or correction insulin.
The theory is, if your basal rate is right then you could go all day without eating and your glucose would remain more or less the same!
How does it work?
An insulin pump allows you to program varying basal rates over 24 hours. Some pumps allow you to change the amount of insulin delivered every 30 minutes – that could add up to 48 different rates in one day, but most people only need about 4 to 6 different rates per day.
Remember: due to the action of quick acting insulin and the way it is delivered by the pump, a change in your basal rate will take effect 90-120 minutes later. For example, the basal rate set at midday will take effect between 1pm and 2pm.
See the following table for a step by step guide on checking your basal rates:
Recommendations for checking your basal rates:
- We would suggest starting with your overnight basal rates
- We would suggest doing these checks a few times on days that are similar to ensure there is a pattern before you make any changes
- Ideally your glucose level at the start of each check should be between 5 and 10 mmol/L (up to 12mmol/l can work)
- Choose a day to basal check when you;
- Have not had a hypo of 3.5mmol/L or below in the past 12 hours
- Have not been significantly more active than normal
- Have not been unwell or are under more stress than usual
- Have not had a significant amount of alcohol in past 12-24 hours
- Abandon if you have a hypo or if your glucose levels go above 12mmol/L and correct
| Time Frame | What to do |
When to check glucose if not wearing a sensor |
|---|---|---|
| Overnight check |
What to do
Begin review if pre bed glucose is between 5-10mmol/L Eat an evening meal that contains 50g or less carbohydrate that you are confident you will count accurately No food or carb containing drinks during the evening No exercise |
When to check glucose if not wearing a sensor 3-4 hours after evening meal Bedtime (if not the same time as above) 2-3am Waking |
| Morning check |
What to do
Begin review if pre-breakfast glucose is between 5-10mmol/L Skip breakfast Eat no food until lunch |
When to check glucose if not wearing a sensor On waking and every 2 hours until lunch |
| Afternoon check |
What to do
Begin review if pre-lunch glucose is between 5-10mmol/L Eat a breakfast that contains 50g or less carbohydrate that you are confident you will count accurately Skip lunch No food or carb containing drinks until evening meal |
When to check glucose if not wearing a sensor 3-4 hours after breakfast Then every 2 hours until evening meal |
| Evening check |
What to do
Begin review if pre-dinner glucose is between 5-10mmol/L Eat a lunch that contains 50g or less carbohydrate that you are confident you will count accurately No evening meal or carb containing drinks Eat a late snack if needed |
When to check glucose if not wearing a sensor 3-4 hours after lunch Every 2 hours until your late snack |
If the glucose levels rise or fall more than 2 mmol/L during the review period this can suggest the basal rates need adjustment.
Adjust the basal rate for the time period 90 – 120 minutes before and up to when the rise or fall in glucose occurs.
Adjust the basal rate by 10-20% or by 0.025, 0.05 or 0.10 units/hr either up or down depending on whether your glucose rose or fell.
Bolus insulin and carbohydrate counting
All carbohydrates consumed should be covered with an insulin bolus unless you are treating a hypo or being more active. The amount of insulin required is calculated by your pump when you enter the carbohydrate in grams into the bolus calculator. If you choose to miss a meal or eat a meal that doesn’t contain carbohydrate you do not need to give a bolus of insulin unless your glucose level is raised at the time of the meal.
You may find that if you have several snacks and insulin boluses in a row, the insulin can build up in the body and work more strongly than intended leading to a low reading later. This is called insulin stacking. If you notice that this is a pattern, please speak to your pump educator.
It is important to count your carbohydrates as accurately as possible. You may find the Carbs and Cals book/app (by Chris Cheyette) useful with carbohydrate counting – see the images shown below. We also offer Carbohydrate Counting Workshops on a regular basis. Please ask your educator to add your name to the list if you feel this would be helpful.

Reviewing your carbohydrate ratios
It is important to ensure your basal rates are correct before you look to make changes to
bolus or correction insulin
Your carbohydrate/bolus ratio determines the amount of insulin needed for carbohydrate eaten at a specific time of the day. In time your bolus ratios are likely to vary across the day. It is useful to be able to check if these are correct.
NOTE: choose a day to do this check when you have not been unwell, stressed, had a hypo in the last 6 – 12 hours, been significantly more active than usual or been drinking alcohol in the last 12-24 hours.
- Check your glucose level pre-meal. You should not have given an insulin bolus within the last 4 hours before this meal.
- Choose a simple meal that you can accurately count the carbohydrates.
- Aim to eat less than 50g carbohydrate or give less than 6 units of insulin so that a normal wave can be used during the check.
- Give your usual insulin to carbohydrate bolus.
- Check your glucose level at 2 and 4 hours after the start of the meal.
| Timing | Target post meal glucose |
|---|---|
|
Timing
2 hour post meal glucose |
Target post meal glucose
Within 2.8mmol/l of pre meal glucose |
|
Timing
4 hour post meal glucose |
Target post meal glucose
Within 1.7mmol/l of pre meal glucose |
If the glucose level is out of target, review your insulin to carbohydrate ratio:
- If the glucose level rises higher than these levels increase the insulin dose by decreasing the carbohydrate ratio by 10-20% or by 0.5 to 1g
- If the glucose levels drop after a meal then reduce the insulin given by increasing the carbohydrate ratio by 10-20% or 0.5 to 1g
If at any stage during the process your glucose level drops below 4 mmol/L, abandon and have a snack. Repeat the process at another time to confirm the result.
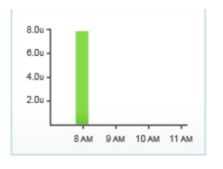
Examples of how to change your ratio following a bolus check…
1 Current insulin : carbohydrate ratio = 1unit:15g
Pre-meal glucose = 5.5mmol/l, 2 hours post meal = 10mmol/l
Increase the amount of bolus insulin by reducing the carbohydrate part of the ratio by 10-20% to 1unit:14g or 1unit:13g
Repeat the process to check whether the change was appropriate
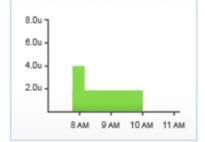
2 Current insulin : carbohydrate ratio = 1unit:8g
Pre-meal glucose = 6.3mmol/l, 2 hours post meal = 4.1mmol/l
Reduce the amount of bolus insulin given by increasing the carbohydrate part of the ratio by 10-20% to 1unit:9g or 1unit:10g
Repeat the process to check whether the change was appropriate
Note: The lower the carbohydrate ratio the more insulin the pump will deliver to cover carbs. The higher the carbohydrate ratio the less insulin the pump will deliver to cover carbs.
We have listed below possible causes of hypoglycaemia and possible solutions to prevent this happening again:
| Possible cause | Possible solution |
|---|---|
| Possible cause Incorrect basal rate |
Possible solution
Check time on pump correct If you use different basal patterns check it’s the right one Too much basal for activity and temp basal needed Consider checking basal if pattern of hypos |
| Possible cause Incorrect bolus given |
Possible solution
Check bolus history Check carbohydrate counting accurate Check timing of bolus for food Consider type of bolus used |
| Possible cause Increased activity |
Possible solution
Consider a reduced temp basal for future activity Consider extra carbs for future activity |
| Possible cause Hot weather |
Possible solution
Consider a different basal pattern for holidays or summer Consider a reduced temp basal if short lived |
| Possible cause Drinking alcohol |
Possible solution
Consider a temp basal overnight (up to 10am) if drinking more than 2 units or Consider carbohydrate bedtime snack Consider reduced bolus at breakfast |
| Possible cause Incorrect insulin |
Possible solution
Always check the following on a new insulin vial; Insulin type, strength, expiry date and how it has been stored. |
- It is important to share this information on correct hypo treatment with close family and friends so that they can assist you, if necessary, to treat a hypo safely.
- Remember to carry quick acting carbohydrate with you at all times for treating hypoglycaemia.
- Please contact your educator if you are having frequent, unexplained hypoglycaemia (more than 2-3 per week) or an episode of severe hypoglycaemia.
How to manage glucose levels which are below target but not hypo
Pre meal/snack:
When you enter a glucose level below target before eating your pump will deduct some insulin from the meal bolus to allow glucose level to rise back into target range. You may choose to give the bolus at the start rather than 10 minutes before.
If it is a large meal or high in fat it will take longer to digest so you may wish to split the bolus and deliver half at the start of the meal and the remaining half halfway through the meal.
In between meals:
Have a small carbohydrate snack to raise your glucose to an appropriate level without covering with insulin.
For example 5g of carbohydrates will raise your glucose level by 1-2mmol/l, 10g by 2-3mmol/l.
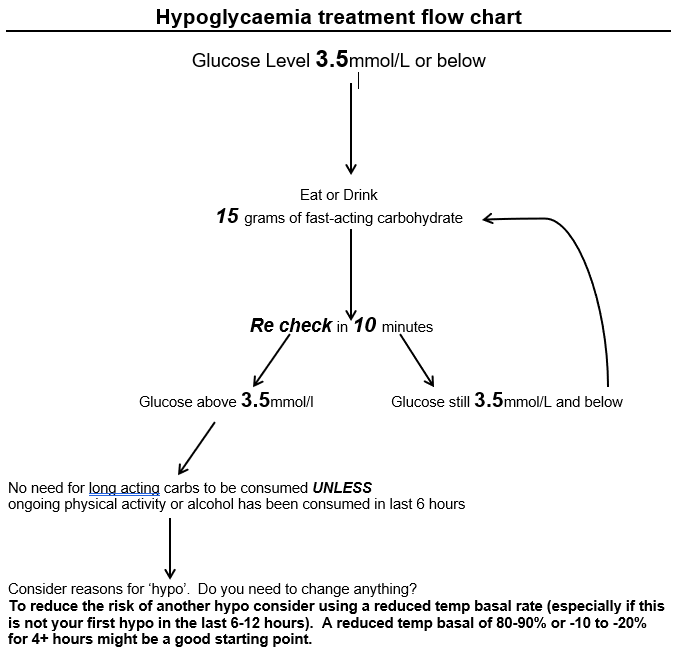
No need for long acting carbs to be consumed UNLESS ongoing physical activity or alcohol has been consumed in last 6 hours
Consider reasons for ‘hypo’. ﻠDo you need to change anything?
To reduce the risk of another hypo consider using a reduced temp basal rate (especially if this is not your first hypo in the last 6-12 hours). A reduced temp basal of 80-90% or -10 to -20% for 4+ hours might be a good starting point.
It is recommended not to correct a high glucose within 6 hours following a hypo and you may have to manually override your bolus dose to achieve this.
Urgent advice: For Severe hypos
Please call the diabetes out of hours (Mon-Fri 4pm to 11pm and 6am to 9am, weekends and bank holidays 6am to 11pm) emergency number
or on 01223 960993 if you (or your carer) require support during or following a severe hypo.
Hyperglycaemia
Occasional highs are not thought to cause significant harm, though they can be frustrating. If you see a pattern with high glucose levels you may benefit from doing a basal or bolus review to identify a possible cause.
| Possible cause | Possible solution |
|---|---|
| Possible cause Incorrect basal rate |
Possible solution
Check time on pump correct If you use different basal patterns are you using the right one? Consider basal review |
| Possible cause Incorrect bolus given |
Possible solution
Check bolus history Check carbohydrate counting accuracy Check timing of bolus for food |
| Possible cause Less active/more stress/ currently unwell/ menstrual cycle | Possible solution Consider using an increased temp basal rate if short-lived |
| Possible cause Cold weather/high altitude/dehydration |
Possible solution
Consider a different basal pattern for holidays or winter Consider an increased temp basal rate if short-lived Ensure adequate hydration |
| Possible cause Insulin |
Possible solution
Always check a new insulin vial for damage, the use by date, strength, correct insulin type. How long has your insulin been out of the fridge, especially if hot weather? |
| Possible cause Blocked cannula/ faulty set |
Possible solution
Are you due a set change? Did your glucose levels rise with a recent set placement? Is the infusion site wet? |
Symptoms of hyperglycaemia
- Thirst and dry mouth
- Nausea
- Urgency to urinate frequently
- Vomiting
- Frequent urination especially at night
- Dry or flushed skin
- Impaired vision
- Poor appetite
- Abdominal pains
- Muscular pains
- Difficulty breathing
- Apathy
- Odorous breath
- Fatigue, weakness
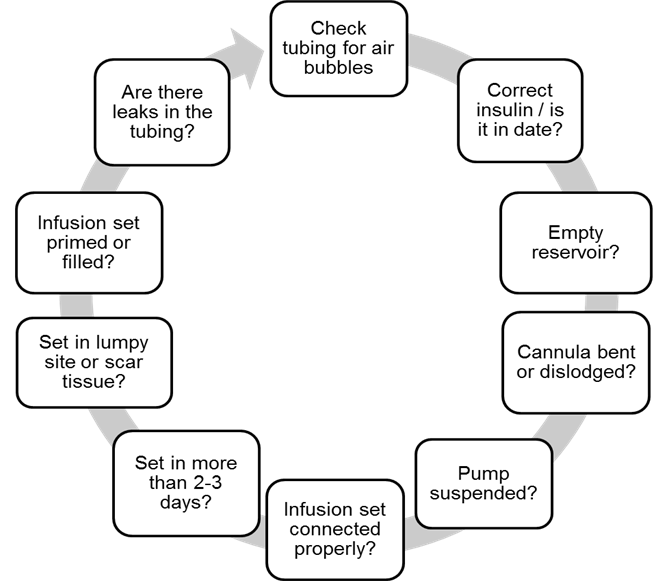
Troubleshooting the pump
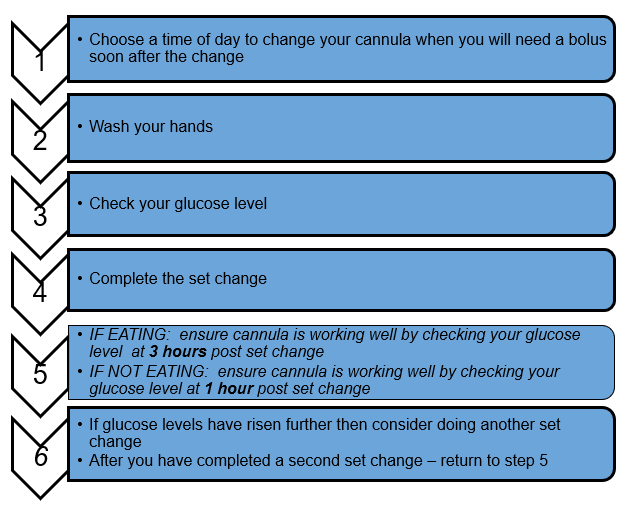
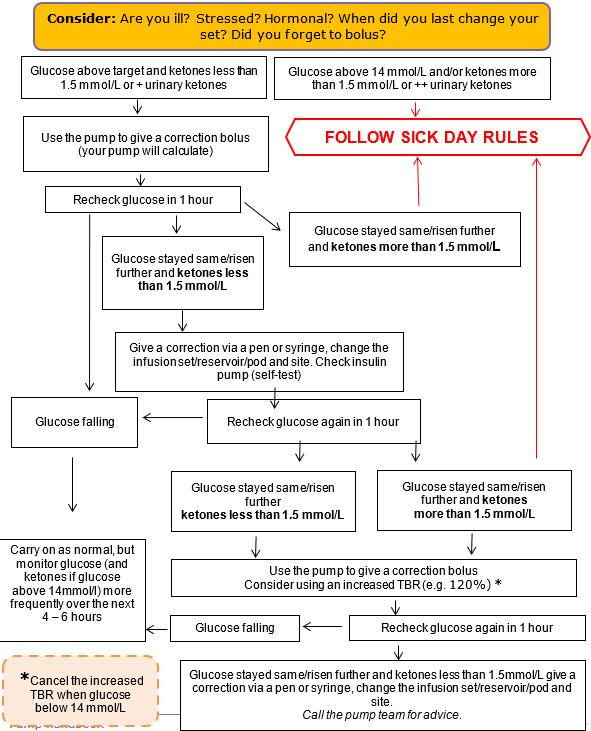
If you are unsure of the cause of the high glucose levels, we would recommend following the guidelines below:
Reduce the risks of hyperglycaemia by:
- Checking glucose levels 4 – 6 times daily (additional checks will be needed when unwell or exercising or pregnant)
- Using a correction bolus pre meals and pre bed as needed
- Changing the infusion set every 2 – 3 days
- Checking the cannula site regularly
- Checking insulin expiry date and use within 28 days if kept at room temperature. Be aware hot temperatures can cause insulin to degrade faster
- Accurate carbohydrate counting
- Using the bolus calculator
If you have forgotten your meal bolus and remembered 2 hours later because your glucose levels are high just take a correction dose rather than cover the carbs
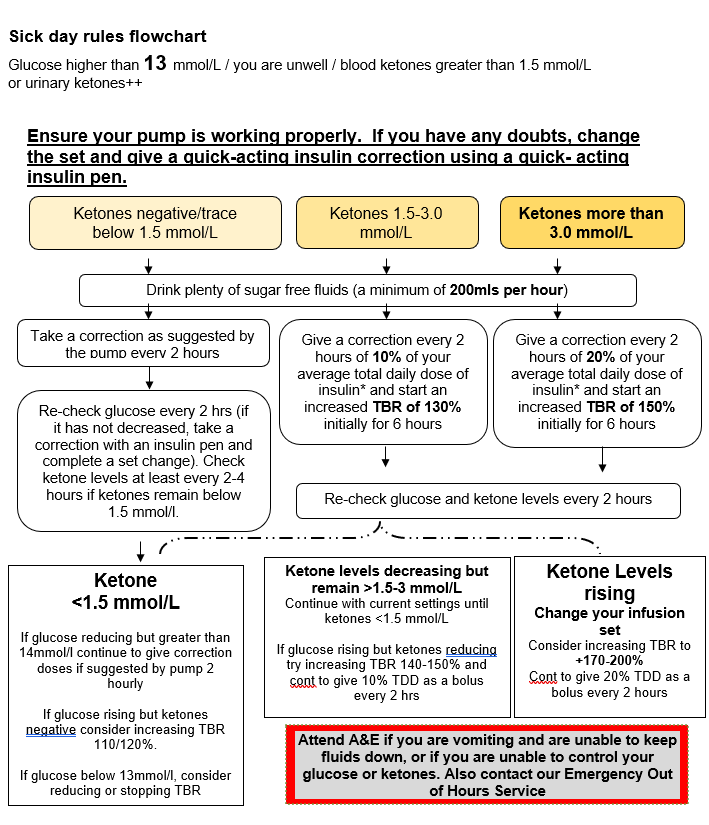
Hyper treatment flow chart
How to work out 10% and 20% of your Total Daily Dose (TDD) of Insulin
1 Work out your TDD – this includes all your basal, bolus and corrective insulin in 24hrs
2 This information can be found in the history menu of your pump (use the 7 day summary).
Alternatively you can get this information from your pump upload
3 An easy way to work out 10% of your TDD is to move the decimal point once to the left…
e.g. if TDD = 34units then 10% = 3.4units
4 An easy way to work out 20% of your TDD is to move the decimal point once to the left and times it by 2… e.g. if TDD = 34units then 10% = 3.4units x 2 = 6.8units
5 Or refer to the table below as an easy guide.
| Total Daily Dose | 10% (additional units) | 20% (additional units) |
|---|---|---|
| Total Daily Dose 20 | 10% (additional units) 2 | 20% (additional units) 4 |
| Total Daily Dose 30 | 10% (additional units) 3 | 20% (additional units) 6 |
| Total Daily Dose 40 | 10% (additional units) 4 | 20% (additional units) 8 |
| Total Daily Dose 50 | 10% (additional units) 5 | 20% (additional units) 10 |
| Total Daily Dose 60 | 10% (additional units) 6 | 20% (additional units) 12 |
| Total Daily Dose 70 | 10% (additional units) 7 | 20% (additional units) 14 |
| Total Daily Dose 80 | 10% (additional units) 8 | 20% (additional units) 16 |
| Total Daily Dose 90 | 10% (additional units) 9 | 20% (additional units) 18 |
| Total Daily Dose 100 | 10% (additional units) 10 | 20% (additional units) 20 |
Carbohydrate for exercise
You may find that altering your insulin isn’t enough to cope with your activities. In some cases you may need extra carbohydrate as well.
The table below details type of carbohydrate based on type of activity, but you may need to work out the amount you need for you activity through practice. You may find need a combination of both type of carbohydrate depending on what you are doing. Have a go at experimenting and see what works best for you.
| Fast release carbs (shorter sessions/events) | Carbs (g) | Slower release carbs (longer sessions/day events) | Carbs (g) |
|---|---|---|---|
| Fast release carbs (shorter sessions/events) Jelly Babies (4 sweets) | Carbs (g) 20 | Slower release carbs (longer sessions/day events) Raisins (30g) | Carbs (g) 22 |
| Fast release carbs (shorter sessions/events) Dextrose (4 sweets) | Carbs (g) 12 | Slower release carbs (longer sessions/day events) Jaffa Cake (each) | Carbs (g) 10 |
| Fast release carbs (shorter sessions/events) Isotonic Gel (each) | Carbs (g) 22-25 | Slower release carbs (longer sessions/day events) Fruit bar (each) | Carbs (g) 15 |
| Fast release carbs (shorter sessions/events) Energy Sports bar (each) | Carbs (g) 25 | Slower release carbs (longer sessions/day events) Cereal bar (each) | Carbs (g) 22 |
| Fast release carbs (shorter sessions/events) Energy powder drink (500mls) | Carbs (g) 45-50 | Slower release carbs (longer sessions/day events) Malt loaf (1 slice) | Carbs (g) 20 |
| Fast release carbs (shorter sessions/events) Gatorade (250mls) | Carbs (g) 15 | Slower release carbs (longer sessions/day events) Banana (medium) | Carbs (g) 15-20 |
| Fast release carbs (shorter sessions/events) Lucozade original (100mls) | Carbs (g) 8.4 | Slower release carbs (longer sessions/day events) Flapjack (50g) | Carbs (g) 30 |
| Fast release carbs (shorter sessions/events) Lucozade Sport (100mls) | Carbs (g) 6.4 | Slower release carbs (longer sessions/day events) Fig roll (each) | Carbs (g) 14 |
| Fast release carbs (shorter sessions/events) Cola (150ml - mini can) | Carbs (g) 15 | Slower release carbs (longer sessions/day events) Oat cake (each) | Carbs (g) 6 |
| Fast release carbs (shorter sessions/events) Apple juice (120ml) | Carbs (g) 15 | Slower release carbs (longer sessions/day events) Bread Roll (50g) | Carbs (g) 25 |
Taking the pump off for exercise
In some situations you may want to take the pump off, e.g. for swimming, contact sports etc. You can do this for up to 60 - 90 minutes. Taking it off for much longer than this will cause your glucose levels to rise. Refer to ‘Taking the pump off’ on page 31 for guidance on this.
Further reading
Hopefully this section has provided you with some ideas, information and advice around managing exercise with your insulin pump. For more general reading around diabetes and managing exercise then you may find the below references useful:
Books
- Type 1 Diabetes – Clinical Management of the Athlete by Ian Gallen
- Getting Pumped! A Diabetes and Exercise Guide for Active Individuals with Type 1 Diabetes by Michael Riddell
Websites
- Runsweet (opens in a new tab)
- Extod (opens in a new tab)
- Insulin-pumps-and-exercise (opens in a new tab)
- Teamnovonordisk (opens in a new tab)
- Excarbs (opens in a new tab)
- Exercise-guidelines (opens in a new tab)
- Ext1d (opens in a new tab) - * need to pay
- Teamwildathletics (opens in a new tab) - * need to pay
Taking the pump off
There may be times when you would like to remove/disconnect from your tethered insulin pump temporarily such as swimming, sex and going on holiday.
Insulin pumps should not be disconnected for more than 1–2 hours unless you follow advice in the table below
| Off the pump for: | What to do: |
|---|---|
| Off the pump for: Up to 90 minutes |
What to do:
Check glucose levels before disconnecting the pump and give a correction if needed using the pump. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. When you reconnect the pump, check your glucose and give a correction if necessary. |
| Off the pump for: Up to 4 hours |
What to do:
Check glucose before disconnecting and give a correction if needed using the pump. At 2 hours after disconnecting use your insulin pen to give a bolus of quick acting insulin equivalent to the amount of basal insulin you have missed. For example if your basal rate is 1 unit/hour give a bolus of 2 units. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. When you reconnect the pump, check your glucose and give a correction if necessary. |
| Off the pump for: Up to 12 hours |
What to do:
Check glucose before disconnecting the pump and give a correction if needed using the pump. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. Followed by either of the below: Every 2 hours use your insulin pen to give quick acting insulin equal to missed basal amount or Take a dose of intermediate-acting insulin (Insulatard, Levemir or Humulin I) at the point of disconnecting that is equal to your basal insulin dose for the next 12 hours. If you choose to reconnect your pump before the 12 hours please run a 0% temp basal for the remainder of time. Finally: When you reconnect the pump, check your glucose and give a correction if necessary. |
| Off the pump for: 24 hours or longer |
What to do:
Check glucose before disconnecting the pump and give a correction if needed using the pump. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. Followed by one of the below: Every 2 hours use your insulin pen to give quick acting insulin equal to missed basal amount. or Take a dose of intermediate-acting insulin (Insulatard, Levemir or Humulin I) at the point of disconnecting that is equal to your basal insulin dose for the next 12 hours. You will need to do this injection twice, approximately 12 hours apart. If you choose to reconnect your pump before the 12 hours please run a 0% temp basal for the remainder of time. or Take a dose of long-acting insulin (Lantus) at the point of is connecting that is equal to your basal insulin dose for the next 24 hours. o If you choose to reconnect your pump before the 24 hours please run a 0% temp basal for the remainder of time. Finally: When you reconnect the pump, check your glucose and give a correction if necessary. |
Please note:
- If you disconnect your insulin pump for more than 4 hours close monitoring of glucose levels is recommended
- There is no need to suspend the pump when disconnected, but should you decide to do this is disconnected for extended durations you may wish to re-prime the line to ensure the tubing is filled prior to reconnecting.
- We would recommend that you discuss any plans to disconnect from the pump with the pump team beforehand and plan ahead where possible. Disconnecting yourself from the pump puts you at a higher risk of developing high glucose levels and forming ketones /DKA.
When out and about
We would encourage you to inform friends, colleagues and family members that you are using an insulin pump and have Type 1 diabetes. There is no need to teach them how to use the pump BUT it is important to tell them what to do in an emergency, and where to find spare supplies.
What your colleagues/friends/relatives need to know
- how to recognise and support you treating a hypo
- where your pump, insulin and hypo supplies are kept
- who to contact for help and when to contact them
Supplies to be kept at work and/or carried with you if more than 1 hour away from home
- Glucose meter/spare sensor (if using)
- ketone meter and/or ketone strips
- spare reservoir and infusion set x 3 (with inserter) or pods
- spare batteries
- quick acting insulin pen
- background / intermediate acting insulin if you are travelling away from home overnight
- copy of sick day rules
- copy of your pump settings
- contact numbers for family, pump team and pump manufacturer
- hypo treatment and extra carb snacks
Travel
Ahead of travelling contact the pump team for a travel letter to support you carrying your insulin pump supplies, sharps and liquids through security. The pump team will arrange this letter free of charge. Please contact us, if possible, 2 weeks prior to your departure.
Insulin pumps can be damaged by being passed through certain types of security screening devices in airports such as X-ray machines and whole body scanners. Airport security staff should provide users of insulin pumps with suitable safe screening options.
Check with your pump manufacturer for guidance about flying with your pump.
If you are travelling to a hot/very cold climate or will be staying at altitude contact your pump team for support as you are likely to need adjustments to your settings.
Remember to change the time on the pump when you reach your destination as well as when you return to the UK. For very long haul travel e.g. to Australia, it may be worthwhile making small changes to the time every 6 hours.
Travel can be very stressful and therefore you may need to run an increased temp basal to ensure your glucose levels are stable. Check glucose levels frequently and correct where necessary. Also remember to drink plenty of fluid.
Extra supplies for travelling
It is recommended that you take twice the amount of supplies (see above re supplies to carry if more than 1 hour from home) that you think you will use. Trips can be extended for reasons beyond your control.
Where possible divide your supplies with someone who is travelling with you or across two bags in case of theft or loss.
You will also need to carry quick acting and background insulin with you for emergency use if the pump fails. Please call the pump manufacturer in the event of failure as they may be able to courier a replacement pump to you depending on where you are in the world.
It may be worth contacting your pump manufacturer well in advance to see if they have spare loan pumps for holidays in case of pump failure.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/