Who is the leaflet for? What is its aim?
You have attended our gynaecology-oncology clinic in the Rosie Hospital, Addenbrooke’s. You will have probably had some tests done prior to this appointment and maybe unsure of what is happening at this stage.
The aim of this booklet is to provide you and your support team with information regarding what has been discussed in clinic.
You will be seen by one of our consultants with a clinical nurse specialist (CNS), together with anyone you may wish to bring with you. They may ask you some questions about your general health and well-being complete a physical examination and an internal examination if required and talk through your options with you.
We aim to answer all of your questions during your appointment but this can be an overwhelming time with lots of information given.
It will outline background information about your diagnosis, surgery options, what to expect before and after your surgery and the recovery process.
If you have any further questions or need further support please do not hesitate to contact us.
Your diagnosis
Being told you have cancer requiring treatment will mean you may experience many different emotions - for example shock, fear, anger, a sense of helplessness and a loss of control. You may not believe this is happening if you don’t feel ill.
You may be frightened about the future and what this may hold for you. These are all normal reactions which may affect you, your family and friends at this time.
We understand this is a very difficult time for you. We aim to keep you and your family informed about your treatments. These will be discussed with you on an individual basis at every stage.
It can be very difficult to take everything in when you are first told about your cancer diagnosis. This booklet is designed to supplement the information given to you by other members of the healthcare team involved in your care.
If you have any concerns or questions about your diagnosis or treatment please contact us. We will try to resolve any issues you may have.
What is cancer?
The body is made up of groups of specialised cells - for example skin, liver, bone, breast cells. Worn-out cells are replaced by new ones. The growth and repair of these occurs in an organised and controlled manner. The right numbers of new cells are produced to replace the old ones.
This process can go wrong. One cell may develop its own pattern of growth and division, producing more and more abnormal cells. These abnormal cells may eventually develop into an abnormal mass of tissue or form a lump. Tumours can be benign or malignant. The pathologist can tell by examining cells whether they are benign or malignant.
Benign tumours are generally harmless. Unless they are causing problems, for example pain, they are generally left alone.
Malignant tumours consist of cancer cells. Some cancer cells have the ability to break away from the original (or primary tumour) and spread to other parts of the body. When these cells reach other parts of the body they can continue to grow and divide to form a new tumour. This is referred to as a secondary deposit or metastasis. Treatment can be offered for both primary and secondary disease.
It is important to remember that cancer is not one disease. There are many different types, which are all treated in different ways. For this reason you may find that other patients are undergoing different treatment to you.
Role of gynae-oncology CNS
This is a nurse who specialises in the care of women with gynaecological cancers and their families. He/she is your key worker and can provide information, advice and support for you and your family, from diagnosis onwards.
This may include:
- Surgery
- Chemotherapy/radiotherapy
- Psychosexual issues
- Support agencies
- HRT and menopause information
- Fertility and infertility advice or information
- Lymphoedema services
- Finance
- Pain and symptom control
- Local and national services
- Hospice care
You may meet your nurse specialist at the outpatient clinic or on the ward.
Contact - 01223 586892
Your CNS can be contacted Monday to Friday 08.00-16.00, we have a voicemail so if no one answers your call please leave a message and we will call you back as soon as possible
If you have any urgent problems over the weekend please contact your out–of-hours GP.
We are always available for advice. Please do not hesitate to contact us.
If you have had surgery recently, advice is available from Daphne ward and Clinic 24 - Gynaecology Assessment Unit, both are located in the Rosie Unit).
Daphne Ward - 01223 257206
Clinic 24 - 01223 217636
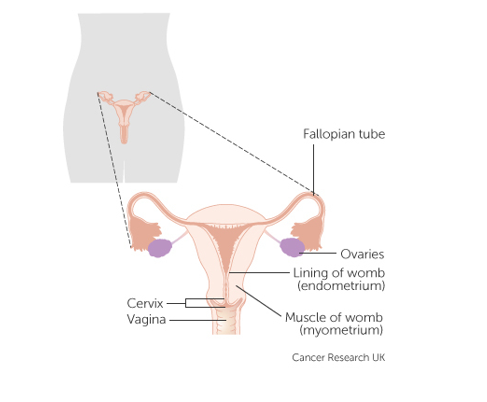
Womb (endometrial) cancer
Womb cancer is a common cancer that affects the female reproductive system it can also be referred to as uterine (uterus) or endometrial cancer. This cancer is more common in women over 40 years of age.
The majority of womb cancers start in the cells that line the womb (The Endometrium) called endometrial carcinomas or adenocarcinomas.
There are other types of womb cancer; uterine sarcoma, clear cell carcinomas and papillary serous carcinomas. Your Specialist Nurse can give you more information on these.
Causes of womb cancer
The cause is unknown however there are factors which may increase a women’s chance of getting endometrial cancer;
- The risk of endometrial cancer increases with age.
- Long exposure to the hormone oestrogen.
- As oestrogen can be produced in fatty tissue, being overweight or obese increases the level of oestrogen in your body. This significantly increases your chances of developing womb cancer.
- Family history - research has shown that daughters of women with womb cancer have double the risk of women in the general population.
- Use of drug Tamifoxen. This is a drug used to treat breast cancer; this risk however is outweighed by the benefits it provides in preventing breast cancer.
- Women who suffer with Poly Cystic Ovary Syndrome (PCOS) are at a higher risk as there are higher concentrations of Oestrogen in the body.
- Diabetes can cause a higher amount of insulin in the body which in turn can raise Oestrogen levels.
- There are a number of rare genetic conditions that may increase the risk of developing womb cancer. The most common is Lynch syndrome.
Clinical guidelines advise that all new womb cancers are checked for Lynch syndrome. This is a hereditary condition which increases the risk of certain cancers, mainly of the womb and bowel (colon). Preliminary screening tests are done as routine clinical care on a womb cancer sample and the results may lead to further investigations. It is important to note that most womb cancers are not due to Lynch syndrome. If your tests indicate that your womb cancer is caused by this or requires further investigation to exclude it, your cancer team will inform you and make a referral for you to the Clinical Genetics service.
The local genetics service can provide a cancer risk assessment and screening advice for you and your relatives. Before a genetics clinic appointment, you may be asked to complete a family history form, as this helps provide accurate advice. At a genetics clinic appointment, your genetics doctor or genetic counsellor will discuss your questions and concerns.
Endometrial hyperplasia (complex atypical hyperplasia)
Endometrial Hyperplasia is a pre-cancerous condition. It occurs when the lining of the womb becomes thicker as a result of increased levels of the hormone oestrogen. This can also occur alongside insufficient levels of progesterone. If this is the case there is a greater risk of development of cancer as cells can exposed to cancerous transformation.
This can be treated by hormonal treatment or a full hysterectomy to prevent the cells developing into cancer.
Treatment
Surgery
The main aim of surgery is to remove as much of the cancer as possible. The surgery you are offered is dependent upon type, size and location of your cancer. Often a hysterectomy is advised which is an operation to remove your womb and sometimes other parts of female reproductive system.
- Both ovaries and the fallopian tubes (Called a bilateral salpingo-oophorectomy),
- The womb and cervix are removed (Called a total hysterectomy),
- The womb, cervix, tissue around the cervix, fallopian tubes, pelvic lymph nodes, part of the vagina and sometimes ovaries are removed. (Called a Radical Hysterectomy). The layer of fatty tissue in the abdomen known as the Omentum (called an omentectomy).
Biopsies and Lymph nodes may also be removed to help with staging of your cancer
- Biopsies and Lymph nodes may also be removed to help with staging of your cancer. Removal of lymph nodes does not improve overall survival but involvement of lymph nodes with metastatic cancer dictates further management appropriately. There are two options-removal of all lymph nodes (lymphadenectomy) from pelvis vs removal of first affected lymph nodes (which can be identified by injecting a dye in the cervix at the start of the procedure and then tracing them during the operation.) This procedure is called sentinel node detection. It helps identify microscopic lymph node spread without having the morbidity of removing the whole lymph node bundle. This procedure is only advocated in high risk/intermediate risk uterine cancers. In the cases where sentinel lymph nodes cannot be identified the surgeon may proceed to do a full lymphadenectomy.
- The surgery can be done by open approach or by laparoscopy or with the aid of a robot. Those who undergo laparoscopic/robotic surgery experience less pain and a quicker recovery and are usually fit to be discharged the day after the surgery. For those undergoing open procedure will need to stay in the hospital for a longer period of time, usually 5 days
Additional treatments
Radiotherapy
Radiotherapy uses high-energy rays to destroy cancer cells. You can have radiotherapy after surgery if the cancer isn’t completely removed or if there is cancer in the lymph nodes. The aim is to reduce local recurrence of the disease. Radiotherapy can be internal or external (Brachytherapy).
Chemotherapy
Chemotherapy is not usually given as the primary treatment for womb cancer, but it can be used after surgery and radiotherapy to reduce the risk of disease coming back. This is called adjuvant chemotherapy.
Chemotherapy uses anti-cancer (cytotoxic) drugs to destroy cancer cells. The drugs are usually given intravenously (by injection into a vein).
Side effects may include; nausea and vomiting, tiredness/fatigue, hair loss, sore mouth, numbness/tingling in hands/feet and increase
risk of infection. There are medications available to help with some of these side- effects.
Hormonal treatment
Hormones naturally exist in the body and help to control how cells grow. The hormones oestrogen and progesterone encourage the womb lining to grow. Your oncologist may suggest a trial of hormone therapy for advance womb cancer or if your cancer has come back. The main treatment is progesterone with the main aim to shrink your cancer.
Your options in regard to chemotherapy and radiotherapy will be explained fully to you by your oncologist and specialist nurse if appropriate.
Clinic follow-up
You might go for a check-up at the surgical outpatients after surgery. You will go to the cancer clinic if you are having or have had chemotherapy or radiotherapy. The surgeon and the oncologist might share your follow up. This means you see the surgeon sometimes and the oncologist at other times.
Contact your doctor or specialist nurse if you have any concerns. You should also contact them if you notice any new symptoms between appointments. You don’t have to wait until your next visit.
Patient led follow-up
This system leaves it to the patient to take the lead in arranging to see your doctor or specialist nurse. When you first finish treatment we arrange the appointment. But once your doctors are happy with your progress you can arrange them yourself.
For example you may want to make an appointment if you have noticed any symptoms that are worrying you or if you have concerns about your health.
Important symptoms to be aware of are;
- bleeding or discharge from the vagina or back passage,
- pain in the pelvic area
- abdominal bloating
- any change in urinary or bowel habits
Telephone: 01223 216251 or 01223 586892
Before your operation
Between the time of your diagnosis and admission to hospital for surgery the gynae-oncology nurses can provide support, advice and information. Everyone has different needs at this time.
Prior to surgery you will be asked to attend for ‘Pre Assessment’, this may be straight after you are seen in clinic or at a pre-arranged later date.
This involves:
- a check of general state of health
- current medication
- a number of routine tests may be carried out - e.g. chest X-Ray, Electro-Cardiogram (ECG)
- blood tests
You will have been given your consent forms to read through. Please sign these and being them with you on the day of your surgery. You will have a brief opportunity to see your surgeon before your operation.
You may be examined again and the side of your operation marked. You will also go through your consent form again with your surgeon.
On the day of your operation (or surgery)
Planned date for surgery: ………………………………………………
Please go to………………………………………………….
At………………………………
On the morning of your surgery please remember:
- Do not eat after (this includes chewing gum) …………………………………………………………………
- You may drink clear water only (non-carbonated and without flavouring) until………………………………
Please do not consume anything after these times as this may cause delay or cancellation to your surgery.
We advise you wear loose and comfortable clothing. We would also advise you to stop smoking for two days prior to surgery.
There will be some waiting involved during the day so we suggest that you bring something to do with you e.g. a book; and if possible for a friend or family member to be with you whilst you wait.
General anaesthetic
During a general anaesthetic (GA) medications are used to induce sleep so you are unaware of procedure/operation and do not feel any pain or move whilst it is being undertaken.
Before having an operation you will be assessed for suitability for a general anaesthetic. This will be done at pre-assessment.
It will either be given as a:
- liquid that's injected into your veins through a cannula (a thin, plastic tube that feeds into a vein, usually on the back of your hand)
- gas that you breathe in through a mask
The anaesthetic should take effect very quickly. You'll start feeling light-headed, before becoming unconscious within a minute or so. Your anaesthetist will stay with you throughout the procedure. They'll make sure you continue to receive the anaesthetic and that you stay in a controlled state of unconsciousness. They will also give you pain-relieving medicine into your veins, so that you're comfortable when you wake up.
General anesthetics have some common side-effects; nausea and vomiting, dizziness, confusion, bruising and soreness. Your anaesthetist should discuss these with you before your surgery and you will be monitored throughout your time in hospital.
Depending on your circumstances, you'll usually need to stay in hospital for a few hours to a few days after your operation.
General anesthetics can affect your memory, concentration and reflexes for a day or two, so it's important for a responsible adult to stay with you for at least 24 hours after your operation, if you're allowed to go home. You will also be advised to avoid driving, drinking alcohol and signing any legal documents for 24-48 hours.
Any further questions your anesthetist or pre-assessment team will be able to help.
General anaesthetic - NHS (opens in a new tab)
After your operation (post-op)
Immediately after your operation you will be transferred to the recovery area in theatre. You will be looked after there until you have woken up from your anaesthetic. You will then return to the ward.
Following your return to the ward you may remain drowsy and sleepy for a few hours.
You will go back to Daphne ward which is located in the Rosie unit on Level 2. This is a 19 bed female general gynaecology ward.
Ward Phone number; 01223 257206
Visiting hours are 15.00-20.00, please contact the ward to arrange visiting outside of these hours.
Post-op care
Pain
The amount of pain experienced following surgery is different for each individual and the operation you have. On the whole, most women experience less pain than expected. You will be given painkillers after your operation, including some to take home with you.
- PCA (Patient Controlled Analgesia)
A PCA is a pump, containing a pain killer that is connected to the patient’s Intravenous line (IV line) that allows you to administer regular pain relief.
You will likely wake up after surgery with a PCA, we will monitor your pain and when it is controlled consider converting to oral painkillers.
- Epidural
An epidural is an injection in the back to help with pain post operatively. If this is an appropriate option for you your consultant or Anaesthetist will discuss this with you prior to surgery.
- Rectus sheath catheter
For those who need an open midline surgery we may keep two catheters inside your abdomen to provide local anaesthetics to the area of the surgery which can be a very effective method of pain control. This is usually removed after 72 hours.
Getting up after your operation
In hospital we will encourage you to mobilise (walk or move around) after your operation as this prevents post-op complications and helps speed up your recovery process.
You will also be required to wear Anti-Embolism stockings (TED stockings) which will help to prevent blood clots. The duration in which you would be expected to wear these post-operatively may vary but will be explained on discharge
Catheter care
During the operation a catheter will be inserted which will remain in for possibly 6-72hrs. It will usually be taken out on the ward the morning after your surgery but this will be decided by your medical team.
Before you go home we will check you are emptying your bladder properly. If there are complications you can go home with a catheter in and appropriate follow-up.
If after removal of a catheter you are initially unable to pass urine or are storing it in your bladder, we may talk to you about the option of self-catheterisation. This is usually a temporary measure.
Wound
Your wound will depend on the operation you undergo. However, dissolvable stitches are used in most operations. Your medical team will inspect your wound during your stay in hospital. Please monitor for redness, swelling, wound becoming hot to touch and discharge. If you have concerns when you are at home please contact us.
At home
In the first few days following your operation a vast amount of ‘internal energy’ will be required by your body to repair itself. This may leave you with only small amounts of energy for the rest of the day. You will find that your body will naturally pace itself. After a particular activity you may find your energy levels are dipping and you require more frequent rests.
It is important you keep mobile, moving around the house and taking regular deep breaths whilst resting to reduce risk of blood clots in the legs and also chest infections and pneumonia.
As the days and weeks pass, your energy store increases so you may be back to your normal pattern. During this time you may find that there are good days when you have lots of energy and days you feel more tired. This is normal.
Housework
In the first few weeks you may find you are only able to do light housework such as dusting and preparing light meals. As your energy levels increase you will be able to incorporate more of your daily tasks into you routine but listen to your body.
Physical exercise
If you participate in regular exercise it is advisable to refrain from this in the first few days to weeks. When your energy levels increase, gentle exercise is encourage but build this up slowly.
Driving
The main requirement for driving is that you feel safe behind the wheel. This involves being able to perform an emergency stop or to swerve very quickly. This is not usually possible in the first few weeks and often takes up to six weeks. When you feel ready we would recommend that you go for a short drive to see how well you can manage.
It is also advisable to check with your insurance company as some impose restrictions on driving for a minimum period of time after surgery.
Insurance
Obtaining insurance just because you have a cancer diagnosis does not mean you will be unable to get insurance.
If you need information on such matters such as life insurance, travel or mortgage insurance visit the Amii website (opens in a new tab) for insurers in your area or Macmillan (opens in a new tab) information can be helpful.
| Time after operation | How might I feel? |
What is safe to do? |
Fit to Work? |
|---|---|---|---|
| Time after operation 1-2 days |
How might I feel?
You are still likely to be in hospital You will have some generalised pain in your abdomen You may have some bleeding |
What is safe to do? Get up, move around, go to the toilet Get yourself dressed Start eating and drinking You may feel tired |
Fit to Work? No |
| Time after operation 3-7 days |
How might I feel?
You may be at home by now Your pain should be slowly reducing and you will be able to move more comfortably You will likely still be tired |
What is safe to do? Go for short walks Continue with exercises you have been given Wash and shower as normal Have a rest or sleep in the afternoon |
Fit to Work? No |
| Time after operation 1-2 Weeks |
How might I feel?
You should experience less pain and your energy levels may start to return to normal Bleeding should have settled or be very little |
What is safe to do? Build up activities slowly Go for longer and more frequent walks Restrict lifting to light loads |
Fit to Work? No |
| Time after operation 2-4 Weeks |
How might I feel?
There will be less pain as you increase moving Energy levels should be returning to normal You should start to feel stronger everyday |
What is safe to do? Continue to build up the amount of activity you are doing to normal levels Could start to consider low impact sport Make a plan for returning to work, possibly on reduced hours or lighter duties |
Fit to Work? Possibly |
| Time after operation 4-6 Weeks |
How might I feel?
Almost back to normal self You may still feel tired and need more rest than you did previously |
What is safe to do? All daily activities including lifting, driving and exercise Have sex if you feel ready Consider going back to work if you do not feel ready talk to your GP or employer about the reasons for this |
Fit to Work? Yes |
Additional treatment/therapies
Gynaecological cancers can be treated with a combination of different treatments. Each case is different and your treatment will be tailored to your individual needs.
This may include:
Surgery
There are several different types of surgery. Your surgeon will discuss these with you based on your individual case.
Chemotherapy
Chemotherapy is a medicine, tablet or given as a drip that kills cancer cells. The aim of chemotherapy may be different according to the stage of disease, with some people not requiring any chemotherapy. Chemotherapy can be used to shrink disease prior to surgery, after surgery to kill any remaining cancer cells or if your cancer returns after initial treatment.
Chemotherapy is given in cycles, with a period of treatment followed by a period of rest to allow your body to recover. There are documented side effects when receiving chemotherapy; however these are dependent on the chemotherapy you receive, the dose and your individual reaction to the drug.
Side-effects may include; nausea and vomiting, tiredness/fatigue, hair loss, sore mouth, numbness/tingling in hands/feet and increase risk of infection. There are medications available to help with some of these side effects.
Radiotherapy
Radiotherapy uses high-radiation beams to kill cancer cells. Although not often used as the main treatment for cancer, but it can be helpful shrinking any secondary tumours or for symptom control. Your oncologist will speak with you about this option and the associated side-effects if appropriate
Hormonal treatment
Some gynaecological malignancies, such as endometrial cancers, are sensitive to hormonal treatment and this can be used to shrink the tumour. Your oncologist will speak about this option if appropriate.
Clinical trials
A clinical trial may be discussed about with you as a potential treatment. This discussion does not commit you to taking part. You can also speak with your doctor to see if there are any clinical trials appropriate to your diagnosis.
Getting back on track
Those who have gone through a cancer treatment describe the first few months as a ‘’time of change’’ – not so much getting back to normal, but finding out what is normal.
Whilst you might have had surgery, you may also need additional treatment and go onto have further treatment such as chemotherapy or radiotherapy. Things may still change during your recovery and as a result of your surgery.
Nutrition
Eating and drinking are an important part of our lives When you have cancer you may become more aware of what you eat and drink. You may wish to find out how diet can play a role in your recovery and future health.
A well-balanced diet is important. For a healthy diet it is important to:
- eat a variety of different foods
- eat at least five portions of fruit and vegetables in one day
- limit sugary food and drinks
- drink water
- reduce your salt intake
- drink alcohol in moderation
- most importantly, enjoy your food.
Fatigue
You may feel tired or worn out, in fact fatigue is one of the most common complaints during the first year of recovery. Rest or sleep may not cure the type of fatigue that you have.
Here are some ideas for coping with fatigue:
Prioritising- Decide which activities are of most value each day and cut out unnecessary tasks.
Pacing - Balance Activity and rest – take frequent breaks. Gentle exercise can help fatigue.
Planning - Consider whether time of day affects your fatigue and avoid unnecessary exertion. Try to space activities out throughout the week and not concentrate all activities into one day.
Posture - Avoid bending and twisting which can be tiring. Try not to sit or stand in the same position for too long without changing your position
Permission - Give yourself permission not to do something that you feel you should and try to delegate to others!
Sex and intimacy
You’ll probably need time to recover and adapt to body changes before you feel comfortable about having sex. How long this takes depends on what feels right for you and your partner. As with all other aspects of cancer, care information needs regarding sexuality differ for each individual.
Partners may also have concerns. Talking openly with each other can have a positive effect on your relationship and make you feel more comfortable with each other.
If you experience difficulties with your sex life and these don’t improve, talk to your doctor or specialist nurse.
Try not to feel embarrassed – they’re used to giving advice on intimate problems. They can give information and advice on different ways of looking at problems or other specialist services.
Support
- Macmillan – Relationship, intimacy and sex
- Cancer Research UK – Cancer and sex
Psychological support
There are a lot of emotions when dealing with cancer. It’s natural to have many different thoughts and feelings after a cancer diagnosis. Some people feel upset, shocked or anxious, while others feel angry, guilty or alone. There is no right way for you to feel.
Being able to talk openly with family and friends can certainly provide a lot of comfort.
Support groups and self-help groups give you the opportunity to share your thoughts and feelings. They can also be a good way to hear how other people affected by cancer coped with their situations. The healthcare professionals caring for you and who know your situation can also be a good source of support.
Many people also use psychological services as a source of support during and after their treatment. Gynaecological oncology Psychological Service (GPS) has been established to provide a woman-centred service for dealing with gynaecological cancer and aims to provide a space for women to discuss adapting to the impact of cancer. The GPS team includes a Psychological Wellbeing Practitioner, Clinical Psychologist and Consultant Psychiatrist who are able to provide a variety of interventions that can offer you an integrated and holistic approach to your treatment, health and wellbeing.
Speaking with GPS can help in many areas, such as helping you make sense of how you have been feeling, adapting and coping with cancer, managing difficult or distressing feelings, learning ways to cope with and prepare for treatment procedures, managing worries and living with uncertainty, finding ways of solving problems and making use of your own strengths and skills, relationship difficulties and moving forward with life after treatment has finished.
If you think you may benefit from these services please speak to your CNS who can complete a referral or explain more about GPS or you can also contact them directly on 01223 216167 (ask for Asmita or a colleague in the GPS service).
Menopause
Some types of cancer treatment cause an early menopause. Types of cancer treatment that can cause an early menopause include:
- surgery to remove the ovaries
- radiotherapy to the pelvis
- hormone therapy
- chemotherapy
Menopause can cause:
- vaginal dryness
- hot flushes and sweating
- feeling sad or depression
- loss of confidence and self esteem
- tiredness (fatigue)
- thinning bones
Hormone replacement therapy (HRT) will reverse most of these effects for some women. It can also help with the emotional effects of menopause. Loss of sexual desire can be a problem. It is important to remember that many factors can influence the loss of sexual desire after treatment for cancer.
There are other ways to help with the symptoms of menopause if HRT is not suitable for you:
- other medications to ease symptoms e.g. gabapentin for flushing symptoms
- Complimentary therapies e.g. homeopathy and acupuncture
- creams and lubricants for vaginal dryness
You can discuss these with your Consultant and your CNS.
Support
- Maggie's, Cambridge | Maggie's (opens in a new tab)
- Alternatives to HRT (opens in a new tab)
- Royal College Obstetrics and Gynaecologists (RCOG) – Menopause and Alternatives to HRT
- Daisy Network (opens in a new tab)
- Menopause – One stop guide, A practical Guide to understanding and dealing with the menopause, Kathy Abernethy
Lymphoedema
Lymphoedema is the swelling caused by a build-up of lymph fluid in the surface tissue of the body. Following some Gynecological cancers and therapy this build up may occur as a result of damage to the lymphatic system due to surgery and/or radiotherapy to the lymph nodes.
Physical systems can include:
- swelling in the legs, ankles and feet
- discomfort and infection
Lymphoedema can be a long-term condition. The symptoms usually respond well to treatment and this means in most cases it can be controlled.
If you notice any swelling you are advised to contact the Gynae-oncology Clinical nurse specialists (CNS’s) for further advice and possible assessment.
Support
- Lymphoedema Support Network (LSN) (opens in a new tab)
- Macmillan – Living with Lymphoedema (opens in a new tab)
Cancer Centre contact details
Consultant gynecological oncologists
Tel: 01223 216251
- Mr Peter Baldwin
- Ms Helen Bolton
- Mr Krishnayan Haldar
- Ms Ciara McKenzie
- Mr Pathiraja Pubudu
- Mr Aslam Shiraz
Gynaecological oncology specialist nurses (surgery)
Tel: 01223 586892
- Hannah Threadgold
- Lindsey Brecken
- Linda Dayal
Medical oncologists
- Dr Joo Ern Ang
- Professor James Brenton
- Dr Christine Parkinson
- Dr Constanza Linossi
- Dr Claire Connell
Secretary: Paola Barbieri - Telephone (01223 217074)
Clinical oncologists
- Dr Li Tee Tan
- Dr Deborah Gregory
- Dr Sarah Prewett
- Dr Simon Duke
- Dr Sarah Smith
Secretary: Paola Barbieri - Telephone (01223 217074)
Gynaecological oncology specialist nurse (chemotherapy)
- Alison Hallett
- Linda Ferguson
- Mihail Lovu
- Gemma Webb
Telephone: 01223 256828
Specialist radiographer
- Katie Bradshaw
- Alexandra Keating
Telephone: 01223 256710
If you call out of office hours, please leave a message on the answering machine and your call will be returned the next working day.
Glossary
Adjuvant Treatment - Treatment – usually chemotherapy or radiotherapy, given after surgery
Benign - A non-cancerous growth within the body, which may interfere with the function of an organ, but does not spread.
Biopsy - The removal of a sample of tissue, which can be examined in a laboratory to find out the cause of an illness.
Cytology - The microscopic examination of cells
Histology - The examination of tissues in order to diagnose the underlying disease.
Intravenous (IV) - Given into the vein, usually by injection so that the substance can work quickly.
Laparoscopy - A minor operation which involves making a small incision in the abdomen so that a small telescope (laparoscope) can be inserted, to enable the abdomen and pelvis to be examined without performing a full laparotomy.
Laparotomy - An operation to open the abdomen.
Lymphatic system - A network of vessels that transport lymph – a clear fluid that comes from the blood and bathes the tissues. It contains water, protein, minerals and white blood cells. The lymph passes through a series of filters (lymph nodes) before it rejoins the blood stream.
Lymphodema - Swelling in the arms or legs which is caused by blockage or damage to the drainage of the lymphatic system. It can happen as a result of some cancer treatments, or from the cancer itself.
Lymph Nodes - Small pearl-like glands that are connected to the lymph system and act as filters to stray bacteria or cancer cells. They also produce lymphocytes which are one of the types of white blood cells in the body. When bacteria or cancer cells reach these nodes, they can become enlarged.
Metastatic/Metastases - The spread of cancer from one part of the body to another by the lymphatic system or by the blood stream.
Omentum - A double layer of membrane that is rich in fatty tissue and lies in front of the intestines, like an apron.
Tumour Markers - Substances produced by some cancers that can be measured in the blood stream. They can be used either to assist in making a diagnosis, or to monitor how the cancer is responding to treatment.
Support
- Gynae-oncology Consultants and CNS team, Addenbrookes – 01223 586892
- Alison Hallet (Gynae-Oncology CNS Chemotherapy) – 01223 256 676
- Maggie Wallace Centre – Addenbrookes Hospital, 01223 249 220
- Macmillan Cancer Support Centre, Oncology outpatients, Addenbrookes Hospital, 01223 274801
- Oncology Centre, Addenbrookes - 01223 216552
Womb Cancer Support (opens in a new tab)
Shine Cancer Support – Cancer support for anyone in their 20s, 30s and 40s (opens in a new tab) or email Shine Cancer Support.
References
- Lymphodema Support Network (LSN) (opens in a new tab)
- Macmillan - Endometrial Cancer (opens in a new tab)
- Macmillan – Living with Lymphodema (opens in a new tab)
- Macmillan – Relationship, Intimacy and Sex (opens in a new tab)
- NHS Choices – General Anaesthetics (opens in a new tab)
- NHS Choices - womb-endometrial-cancer (opens in a new tab)
- Alternatives to HRT (opens in a new tab)
- Royal College Obstetrics and Gynaecologists (RCOG) – Menopause and Alternatives to HRT (opens in a new tab)
- Royal College Obstetrics and Gynaecologists (RCOG) – Recovering well (opens in a new tab)
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

