What is a thoracotomy?
A thoracotomy is an operation to open the chest to explore, inspect and operate on a chest organ [lungs/ heart/ trachea (windpipe)/ oesophagus (food pipe) etc].
Why is my child going to have a thoracotomy?
There is an area or organ inside your child’s chest which is either diseased or malformed and needs removal or surgical correction.
Before admission for surgery
Before surgery takes place the following will occur:
Pre-operative assessment
You will be asked to complete a ‘health screening questionnaire’ when your child is added to the waiting list; this will be completed immediately after your appointment if your child was seen in one of our clinics at Addenbrooke’s or, over the telephone if your child was reviewed in one of our outlying clinics.
Blood tests
Blood tests will be required and these are taken within 4 weeks of the operation date.
Admission to hospital
You will be asked to bring your child to one of our children’s wards. For most children this will be early in the morning on the same day as the operation but occasionally, this may be one day prior to surgery if your child has an underlying condition which means they need monitoring before surgery. You will be met by nursing staff and seen by your doctors and anaesthetist. Whilst you child is in hospital you will be able to stay with your child overnight if you wish. You can also be present while your child goes to sleep for their operation, and in the recovery area where he/she wakes up.
The operation
- Thoracotomy surgery can be carried out as an ‘open’ or ‘thoracoscopic’ operation. Your surgeon will discuss which procedure is planned for your child.
- An ‘open’ operation involves making an incision (‘cut’) along your child’s side and back so that the chest organs can be clearly seen. In some cases part of a rib needs to be removed, but the rib will grow back over the following few weeks.
- In some cases it is possible for the surgery to take place ‘thoracoscopically’ (keyhole surgery). This involves three or more small (approximately 1cm each) openings being made in the chest. Through these holes, special tools (‘instruments’) are used to perform the operation. This is all visualised on a TV screen by a miniature camera which is inserted through one of the key holes. The actual operation which takes place is the same as the traditional ‘open’ procedure; it is only the way in which we get to the organ which is different.
- Whether a thoracotomy is carried out as an open or thoracoscopic procedure, many children will have one or two chest drains inserted at the end of the operation. (See below).
What is a chest drain?

The end of the drainage tube is placed into a collecting bottle with the tip submerged in water. The water acts as a valve, stopping air from re-entering the space where the drain is sitting. Sometimes suction will be used to encourage drainage.
An x-ray will be taken of your child’s chest to check the state of the lung and the drain’s position. To prevent the drain from falling out a stitch and dressing will be used to hold the tube to the skin.
Removal of the chest drain usually takes place two to five days after the operation. Chest drains are usually removed on the ward by your nurses or doctor.
What are the risks of surgery?
Risks related to thoracotomy surgery are rare. Risks include:
- Bleeding
- Infection
- Pneumothorax (i.e. an air leak from the lung into the chest)
- Lymph leakage (very rare)
- Nerve damage (very rare)
These risks will be discussed with you by your surgeon.
After the operation
- You will be able to be with your child as soon as possible after the operation.
- Children are often transferred to the children’s high dependency unit for close observation after surgery. Most children will then be transferred back to the ward within 24 hours.
- Children are often able to start eating and drinking again on the day of the surgery. Until this time your child will have a ‘drip’ to provide their fluids and prevent dehydration.
- Your child will require pain killers after the operation and your doctors and nurses will discuss this with you. Pain killers can be given through a special drip, as suppositories and/or as medicine.
- Your nurses will monitor your child and their chest drain. Whilst your child has a chest drain it is very important that he/she does not mobilise without the nurse first being told. This is to prevent complications developing.
- After surgery your child will be encouraged to do deep breathing and coughing exercises if they are at an age where they can follow commands. It is important that these are done as they help to prevent a build-up of phlegm. If you feel your child is unable to cough due to pain please ask the nursing staff for some more pain relief as the breathing and coughing exercises are essential for a quicker recovery.
- Children will be encouraged to mobilise from day one after surgery; see section on ‘mobilisation after surgery.’ If your child has any difficulty with moving with support from the nursing team or carers or, any difficulty with coughing, a physiotherapist will review your child as the earlier children start moving around the lower the risk of developing complications associated with surgery.
Mobilisation after surgery
Once your child has been reviewed by the surgical team on the day after surgery and assessed to be ready, we will aim to get your child out of bed and moving around on day one after surgery.
For younger children this will initially include sitting out on your knee or, sitting in a chair for those that are older and thereafter, increase walking and playing every day. Our aim is to get your child as close to how they were before coming into hospital as soon as possible.
For babies and very young children that need to be lifted, avoid lifting up underneath their armpits, instead, scoop underneath their bottom and around their backs. This lifting method should be used for one to three weeks post op.
Encourage regular use of arm, or shoulder stretches at least two to three times per day. If your child is unable to follow commands, then these exercises can be carried out through play or with your assistance. All of the following exercises will stop your child from becoming too stiff and allow them to take bigger breaths.
Shoulder Abduction
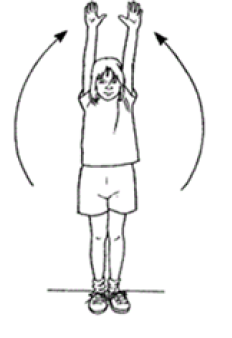
Standing/sitting
Lead with thumbs; lift arms out to the sides as high as possible. Keep elbows straight. Try to touch arms to the sides of the head as pain allows. Slowly lower arms back down. Repeat this exercise 10 times
Trunk Rotation

Twist at the waist, turning the shoulders. Use arms to help twist. Hold this position for 3 seconds. Slowly go back to the starting position. Do this exercise again, twisting at the waist and turning your shoulders to the other side. Repeat this exercise 5 times.
Trunk Side Flexion

Have your child stand/sit with arms by their side. Slide their hand down their leg so the back bends sideways.
Hold position for 3 seconds Return to middle.
Repeat 5 times.
Shoulder Flexion

Raise the arm on the operated side as far as able above the head. Try to keep the elbow straight. Slowly lower arm back down.
Repeat this exercise 10 times.
Looking after your child at home
Stitches
The stitches used in the wound itself are dissolvable. Some stitches used to hold chest drains in place are removed at the same time as the chest drain but others (called ‘purse string stitches’) need to be removed seven days after the chest drain is removed. Your nurse will tell you which type of stitch your child has and where you need to go to have a purse string stitch removed (for example, at GP surgery/on ward).
Pain
Your child may have some discomfort and should be given the pain killers supplied regularly.
Bathing
Your child can have showers but baths are not permitted for five days.
PE/exercise
- Children who are of an appropriate age should continue to perform the breathing exercises, coughing exercises and physical exercises as described above.
- It is important you continue to actively encourage your child’s walking/moving around at home. Aim to exercise at a level that makes them slightly short of breath; this includes crawling and tummy time.
- Your child should be kept off all PE for two to three weeks, depending on their comfort level.
- In the first six weeks after surgery your child:
- Must NOT perform any heavy pulling or pushing tasks with the arm on the affected side.
- Must NOT hang from climbing frames
- Must NOT participate in contact sports
- Children should avoid activities which involve heavy lifting, pulling or pushing through the operated side for 6 to 8 weeks after surgery.
Follow up arrangements
Your child will be reviewed in the outpatient clinic. This may be between two and six months after the operation depending on the reason for the surgery having been undertaken. The doctors/nurses will let you know when your child is due to return for the check up and the actual appointment will be sent to you in the post.
Chaperoning
During your child’s hospital visits he will need to be examined to help diagnose and to plan care. Examination, which may take place before, during and after treatment, is performed by trained members of staff and will always be explained to you beforehand. A chaperone is a separate member of staff who is present during the examination. The role of the chaperone is to provide practical assistance with the examination and to provide support to the child, family member/carer and to the person examining.
Contact Details
If you have any questions please call:
Your nurse specialist ………… 01223 586973
The ward ……………………………
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

