Hybrid Closed Loop (HCL) system
This has been written to help you get the most from using your Tandem T:Slim X2 with Control IQ insulin pump with continuous glucose monitoring (CGM) in hybrid closed loop (HCL): Control IQ.
Information is accurate as of September 2025
Diabetes insulin pump team contact numbers
Please contact the team if you need advice regarding your diabetes. You can leave a voicemail on one of the numbers below (the answerphone is checked regularly Mon-Fri office hours)
Diabetes specialist nurses: 01223 348790
Diabetes specialist dietitians: 01223 348769
Urgent advice: In an emergency please call the Type 1 emergency out of hours service. If you do not have this number, please ask your diabetes educator.
Alternatively, you can use the Diabetes eConsult service
To contact a diabetes educator, please use MyChart (preferred route of contact)
- Click on Messages
- Then click "ask a question"
- Then click "New question for your clinical team"
- Choose the appropriate option then choose Diabetes Educator
Or use this email address: cuh.diabeteseducator@nhs.net
If using email, you must ensure the subject of the email includes: full name, date of birth and hospital number.
All messages are checked: Mon/Wed/Fri. It is for non urgent enquiries; allow up to 5 days for a reply if using the eConsult service. Please ensure you have uploaded your pump to Glooko/Tandem Source (if applicable).
For any technical queries please contact Air Liquide/Tandem directly on the number below:
0800 0121 560
Please note that the pump company cannot give medical advice, they can only offer technical support.
How do these systems work?
A Hybrid Closed Loop (HCL) system is made up of 3 parts:
- An insulin pump: Tandem T:Slim X2
- A continuous glucose monitor (CGM); aka sensor– Dexcom G6/G7
- An algorithm that takes data from the pump and the sensor and adjusts some of the insulin delivery automatically. This mode is called “Control IQ”.
Hybrid closed loop may also be called Automated Insulin Delivery (AID) systems.
Your pump will deliver insulin in 3 ways:
- Basal: an ever-changing amount of insulin according to the glucose information received from the CGM. Basal delivery may suspend if the hybrid closed loop system predicts below target glucose levels.
- With carbohydrates: you will need to give a bolus of insulin for carbs with pre-programmed insulin to carbohydrate ratios
- Corrections: either suggested by the pump (delivered by the user) or as auto-corrections when sensor glucose is predicted to be above 10 mmol/L and basal insulin has reached max basal delivery. This occurs in the background. This automatic correction is calculated as 60% of the total correction bolus based on your preset correction factor/predicted CGM readings and insulin on board (IOB).
The system is able to keep your glucose levels within target range when things are stable but it is not as responsive to rapid changes to glucose levels with exercise or after carbohydrate. You will still need to give timely bolus insulin for carbohydrates, carbohydrate count well, adjust for exercise and be aware of active insulin on board when exercising or treating hypoglycaemia.
Tandem T:Slim X2 in Control IQ uses CGM data to adjust your insulin delivery
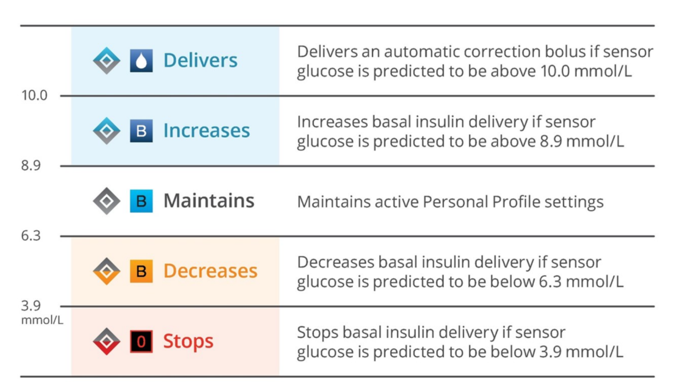
The system aims to maintain your glucose level between 6.3 and 8.9 mmol/L
What settings can I adjust on the pump?
The Tandem T:Slim X2 with Control IQ is highly customisable; the following settings can be adjusted:
- Carbohydrate ratios
- Correction/sensitivity factors
- It is recommended that this setting be optimised to enable the algorithm to work more aggressively without causing more hypos.
- Your correction factor on Control IQ may be much stronger than you would expect. Your diabetes team can help you decide on changes if you need support.
- Basal rates
- Up to 6 personal profiles are possible. e.g. you can set a profile for: work; menstruation; day off; active; weekend etc.
- It is advisable that you aim to optimise a single personal profile before creating a second profile. If you need any support with creating a second profile, consider discussing this with your diabetes team.
- Sleep activity mode
- Aims for glucoses between 6.3-6.7 mmol/L
- Basal rates will increase if glucose level predicted to rise above 6.6 mmol/L
- Auto corrections stop
- Exercise activity mode
- Aims for glucose level of 7.8-8.9 mmol/L
- Basals are reduced if glucoses predicted to fall below 6.7 mmol/L
- Basal is suspended if glucose is predicted to fall <4.4 mmol/L
- Weight
- Total daily dose
Getting started
Initially this technology may take more of your time and attention as you get used to it and while you work on getting your settings optimised. Some parts of using the system will be very familiar to you such as giving a bolus of insulin to cover carbohydrate food and drink, whereas other aspects might feel very different such as treating a hypo and giving corrections. Consider clearing your diary as much as possible for the first week or so, to give yourself time to adapt to the new approaches.
You may find that there are more alerts initially – these might be hypoglycaemia alerts, lost sensor alerts or the system requesting attention and further information. Be patient and keep in contact with your educator – it can take a few weeks to really understand how the system operates and to see if adjustments to your pump settings are needed.
Top Tips for using Tandem T:Slim X2 in Control IQ
- Get the basics right
- Carbohydrate counting – work to get this as accurate as possible.
- If you need further support, consider booking onto one of our carbohydrate counting workshops or completing the DAFNE closed loop essentials course (see further resources section for details)
- Bolus for carbohydrates 15 minutes before carbohydrate food and drinks (unless you use Lyumjev or Fiasp; in which case you can bolus just before eating and drinking carbohydrate.) – see point 3 for more information.
- Regular set changes – every 3 days if using a Teflon cannula (e.g. Autosoft 90) and every 2 days if using a steel cannula (Tru-Steel).
- Rotate cannula sites to avoid impaired insulin absorption if the same site is over-used or lumpy.
- Make sure your insulin has not been out of the fridge for more than 28 days.
- Calibrate your CGM if there is more than a 20% difference between your sensor and blood glucose value.
- Check your sensor is not dropping/losing signal to the pump. The easiest way to do this is by uploading your pump to Glooko.
- If you lose signal; ensure the pump is worn with the screen facing outwards
- Try to keep the pump closer to your sensor
- Try to keep the pump on the same side of your body as the sensor
2. Correction factor: ptimisation of this setting is recognised to be very important in the Control IQ system. If you suspect your correction factor is not right for you, please get in touch with the diabetes team.
- Meal bolus timing: if you are using NovoRapid or Humalog, then give the bolus 10-15 minutes before eating/drinking carbs so that the insulin and carbs are absorbed at the same time and the bolus insulin will cover the carbs most accurately. If you are using Lyumjev or Fiasp, then bolus just before eating and/or drinking carbohydrate. Mis-timed boluses can lead to high post meal/snack glucose levels followed by hypoglycaemia as the HCL may over-compensate if it detects a rapidly rising glucose.
3.1 Missed boluses
- If less than 30 minutes have passed: bolus for all the missed carbs
- If 30-60 minutes have passed: bolus for half of the missed carbs
- If 60+ minutes have passed: give a correction for the current glucose only
3.2 Extended bolus
- This type of bolus is particularly useful for high fat and/or protein meals, or those that contain slow-digesting carbohydrates.
- Here's how an extended bolus can help:
- Meals high in fat and protein (e.g. pizza, rich pasta dishes, heavy curries, cheeseburgers) can cause a delayed and prolonged rise in blood glucose, sometimes lasting for many hours.
- A standard bolus given upfront for such a meal might cause a hypo before the glucose from the meal fully absorbs. This could be followed by a significant high glucose later as the prolonged digestion continues.
- An extended bolus allows you to deliver a portion of the meal insulin upfront and the remaining portion gradually over a set period. This helps to match insulin delivery more closely to the prolonged glucose absorption, leading to a smoother post-meal glucose curve. For very prolonged or high-fat/protein meals, an extended bolus can provide a more proactive and consistent insulin delivery over a longer duration, potentially preventing glucose from climbing too high in the first place or reducing the need for multiple hourly auto-corrections.
- How to use Extended Bolus with Control-IQ:
- A good starting point would be setting a 60% upfront bolus (“deliver now”; with the remaining 40% set as “deliver later”
- Try a duration of 2 hours to start with. Note at present you can only extend up to 2 hours in 30 minute increments (correct at the time of writing).
- Trial and Error: Finding the perfect extended bolus settings for different meals often involves some trial and error and careful monitoring of your glucose trends. Because extended bolus duration is limited to up to 2 hours, you can adjust the insulin split—for example, using a 70/30 ratio between immediate and delayed doses.
4. Hypoglycaemia:
- Generally, less hypo treatment is required in hybrid closed loop systems. It would be worth reviewing sensor arrows and insulin on board to guide the amount of hypo treatment required, if any.
- Consider the cause of the hypo: e.g. unplanned exercise; overestimated the carbs?
- It’s also worth noting that these systems will alert you that you are heading towards a hypo; the system will already have shut down insulin delivery to avoid the hypo and you should try to resist acting too quickly with carbohydrate top ups which could result in overtreatment and rising above target. The low alert soon alarm is a prompt to monitor your glucose more carefully and see if the system is levelling the glucose out or if you do need a small carbohydrate top up (3-7g) as well.
- Try not to take a 10g carb snack after a hypo
- Consider using a blood glucose meter to check your levels to avoid over treating hypos
5. Managing hyperglycaemia: remember your system is designed to keep your glucose within target glucose range; if your glucose levels are running above this range for more than 2 hours and not coming down with corrections then it is likely your set / cannula has failed and should be changed. Ensure you check your ketones if this does occur.
6. Managing illness and ketones: the HCL function does not manage well when ketone levels are raised (e.g. during illness). It is not able to meet the need for increased insulin requirements fast enough. For periods of illness where ketones are present (greater than 1.5mmol/L) turn off Control IQ and follow the sick day rules: DTNSDRPUMP (opens in a new tab)
7. Plan ahead for physical activity.
- Turn on the Exercise activity 60-120 minutes before planned exercise to reduce the insulin on board for starting exercise.
- You may still need to supplement with small amounts of slow acting carbs every 10-30 minutes dependent on the intensity of the exercise
- Avoid pre-loading with carbohydrate before exercise as this results in a rise in blood glucose that activates the automated basal/automatic corrections to increase which could then lead to hypoglycaemia.
- If you would like to halt the auto corrections for 60 minutes:
- Give a 0.05 unit manual bolus just before starting the exercise.
- You can continue to do this if you wish for longer bouts of exercise.
- For those who regularly undertake exercise; it is advisable to create a new personal profile with weaker basal rates/carb ratios and correction factors.
- Conversely, if you undertake exercise that causes high glucose levels (e.g. competitive sports; sprints; hill cycling) you can consider creating a new personal profile with stronger basal rates/carb ratios and correction factors.
8. Managing alcohol – there is a higher risk of hypoglycaemia if alcohol has been consumed. The following advice does not have a formal research base. You should use your own experiences with how alcohol affects you when making decisions about glucose and alcohol.
- Consider turning on exercise activity 90-120 minutes before consuming alcohol to raise your glucose targets. Keep exercise activity on for the whole duration of drinking alcohol; and all night (while asleep).
- You can consider giving a 0.05 unit manual bolus every 60 minutes to prevent automatic corrections.
- Carb count your alcoholic drinks and enter half the amount of carbs into your pump (so you get half the amount of insulin).
- You can also consider a duplicate personal profile (named “alcohol”); where your overnight basals are reduced (try 30-75% reduction), and your correction factors are weakened (increase the correction factor by 50-100%).
Examples:
- Usual basal rate: 1.0 units/hr
- Alcohol basal rate: 0.25-0.7 units/hr
- Usual correction factor: 3.0 mmol/L
- Alcohol correction factor: 4.5 – 6.0 mmol/L
- Ensure your hypo alarms are turned on; you may want to consider increasing the low alert alarm to 5.0 mmol/L for overnight.
- Continue exercise activity the morning after alcohol if you have had a lot to drink the night before.
- If eating: consider a reduced carb bolus to prevent hypoglycaemia. E.g. start with a 20% reduction in the carbs you enter into the pump. If you hypo despite this, consider a 30-50% reduction in the bolus.
- Example: A pasta meal of 60g carbs while on a night out drinking alcohol; enter 48g into the pump (20% reduction).
- Alcohol correction factor: 4.5 – 6.0 mmol/L
9. Suspending the pump – you should suspend the pump if disconnecting for longer periods of time to avoid the system accounting for insulin not delivered. E.g. showers, baths, swimming, sex etc.
10. Avoid overriding the system – you may have been tempted in the past to add pretend carbohydrates to your pump to bring a high blood glucose down when corrections haven’t worked well enough. This approach does not work in HCL and will increase the risk of a hypo.
11. Use the Sleep Activity feature: schedule this to turn on and off automatically so the algorithm helps you to wake up at around 6.1mmol/L.
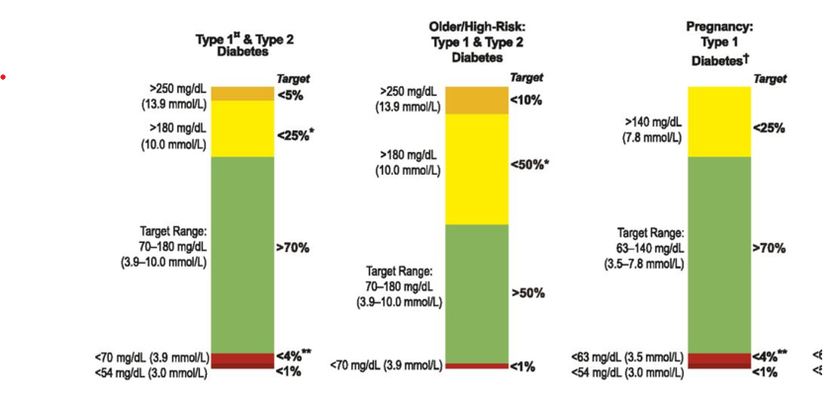
12. Review the data – you can get a lot of data when using HCL. Over time this will become more familiar and useful to you. Your educator can help you interpret what the reports mean and how to make adjustments. The reports also present your glucose data in a different way; in addition to predicted HbA1c (GMI) you will get time in range. You are aiming for at least 70% time in range (3.9-10 mmol/L) with less than 4% below 3.9mmol/L and less than 1% below 2.8mmol/L. Every 1% more time in range is the same as another 15 minutes with blood glucose in range so even small changes make a difference to your health.
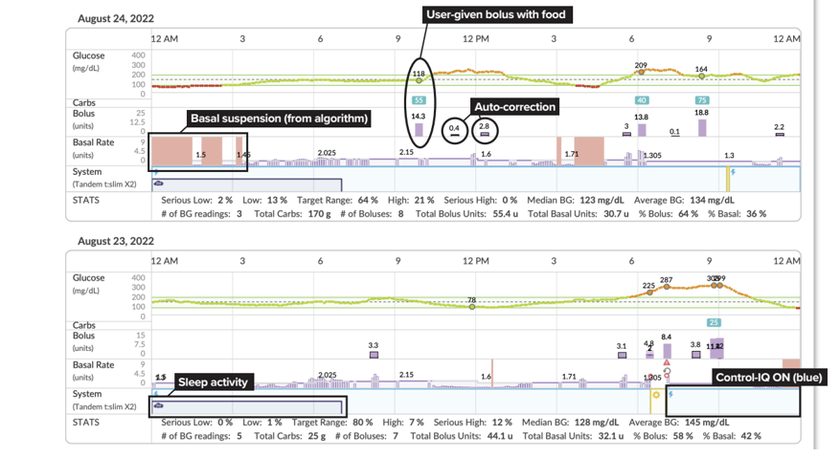
If you are using the T:Slim X2 mobile app, you will be uploading data to Tandem Source. You can find more information about Tandem Source here: What is tandem source (opens in a new tab)
If you are using the T:Slim X2 mobile app, you will be uploading data to Tandem Source. You can find more information about Tandem Source here: what-is-tandem-source (opens in a new tab)
12. Update your basal rates, correction factors and carbohydrate ratios over time if the following changes:
- Your weight
- If you have lost or gained weight, don’t forget to update your weight in your pump (in the Control IQ settings).
- New exercise regimens
Additional resources
- Control IQ training modules (opens in a new tab)
- Quick info sheet; how to view current status of your pump: CIQ status (opens in a new tab)
- Making Diabetes Easier: t:slim x2 mobile app (opens in a new tab)
- Making Diabetes Easier: What is Tandem Source (opens in a new tab)
- Pump sick day rules (opens in a new tab)
Uploading your pump
Uploads can be carried out on Glooko. (ProConnect code: ukaddhos)
Or alternatively please use the Tandem Source software (opens in a new tab)
Carb Counting Workshops
The workshops are held face to face and virtually; to book on please email the Nutrition and Dietetics Admin Co-Manager.
DAFNE closed loop essentials
- The focus of the course is keeping safe using closed loop, so people are aware of what closed loop can and can’t do, and the user input required to use closed loop effectively.
- 4-6 hours of self-directed online learning
- The course content is not specific to a particular pump and is not designed to cover specific pump functions other than the basics.
- Participants will require access to a computer, laptop or tablet and a WIFI connection in order to complete the course.
- You will learn:
- How HCL works
- Carb counting
- Checking your settings
- Hypos and HCL
- Sickness and ketone guidance for HCL
- Going back to injections
- To access the course message the diabetes educator team using the eConsult service (page 1)
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

