
What is talipes or clubfoot?
Talipes or Clubfoot is a condition present at birth in which one or both feet are turned in compared to the normal position. The full medical term used to describe this condition is Congenital Talipes Equino-Varus (CTEV).
- Congenital - present at birth
- Talipes - the foot or ankle
- Equino - the foot points downwards from the ankle
- Varus: - the heel bone is tilted in (when viewed from behind).
The condition may affect one (unilateral) or both feet (bilateral). The affected foot and calf are often smaller than normal. This might not be obvious if both feet are affected.
Clubfoot can be classified in to four different categories: structural, positional, complex/atypical and syndromic. Structural is by far the most common and for the purposes of this leaflet, we will be referring to the structural clubfoot. Additional leaflets are available for both positional and atypical clubfoot.
What causes Clubfoot?
In the majority of cases, there is unfortunately no known cause for clubfoot. The Clubfoot posture / position affects the development of the shape and orientation or positioning of the small bones of the feet as the baby develops in the womb. One of the small bones of the foot is usually remains rotated compared to the position expected in a normal foot. This causes the foot to develop in the turned in position and results in the soft tissues (muscles, tendons and ligaments) on the inside of the foot becoming short and tight which further rotates the foot in.
There are certain factors which can make clubfoot more likely, such as a family history of the condition, too much or too little amniotic fluid in the womb, restrictive bands within the womb, twins / triplets, or something as simple as the position of the baby. Occasionally clubfoot can be associated with other chromosomal or genetic syndromes; however, this is very rare and would most likely be discussed with you at your antenatal appointments.
Clubfoot affects approximately 1 in a 1000 live births in the UK and is twice as common in boys as girls. It is about 50:50 whether both feet are affected or just one is affected.
There has been a small link found between foot problems in children and clicky hips, so at Addenbrooke’s we routinely refer all children diagnosed with foot problems at birth for an ultrasound scan of their hips as part of their assessment.
What is the treatment for clubfoot?
The internationally recognised best treatment for clubfoot is the Ponseti technique. This aims to correct the child’s foot position to create a pain free functional foot with the minimal amount of surgery. The appearance of the foot and the position in which it is held will improve considerably. However, bearing in mind the smaller foot size and reduced calf bulk associated with the condition, the technique is not able to make the foot completely normal, the foot will always be a corrected clubfoot. It is a highly successful management, if adhered to properly and is successful in over 90% of cases. This is the treatment approach used by Addenbrooke’s and is managed by the paediatric orthopaedic team.
There are several stages of treatment with the Ponseti technique and this leaflet will aim to describe each stage. The first stage involves a series of gentle stretches to the foot or feet with the new position held in place by plaster casts. The aim of the casts is to move the foot in the opposite direction to its starting position which takes on average five casts. Once this has been achieved, the majority children will then need a small procedure and further casts to free up the achilles tendon at the back of the heel and hold this position whilst it heals. The final stage of the treatment will involve your child wearing boots attached to a bar to brace and therefore maintain the corrected position of the foot. This is for 23/24 hours a day for the first three months, then night and nap time until he or she is five years old.
When will the treatment start?
If your child is born with this condition, a referral to the paediatric orthopaedic team will be made for your baby, and an appointment will be arranged in the paediatric outpatient department. This will normally occur between two and four weeks after your baby is born (or two to four weeks after due date if your baby is born early). The treatment will be discussed with you at that time, and the Ponseti casting is normally started straight away in this appointment.
What does each stage involve? 1 st Stage: Casting

The casting process is done in the plaster room where a member of the paediatric orthopaedic team will carefully position your child’s foot whilst the plaster technicians apply the casting material. The casts go from toes to groin and the knee will be bent to approximately 90 degrees to reduce the chance of the casts slipping down the legs. The casts are changed every week, with an improved position achieved with each cast until the foot is corrected. Several weekly appointments will be required for this stage and these will be arranged for your child by the team. We ask parents to soak the casts prior to each appointment in order to help with the removal process in clinic. Once the new cast is complete it is helpful to take a picture so you are sure of the position of the toes, which we ask you to check daily in case the cast has slipped. Slipped casts carry the risk of causing blisters or pressure areas to the foot as well as adversely affecting the position of the foot so need to be removed promptly

How can I help?
We do not think that the casting process is painful for babies as the foot is not forced into each position, but merely guided through a gentle stretch. However, babies can be unsettled during the casting process as they may be intolerant of handling and their movement is restricted as they are held still to allow the best cast position to be achieved. It is often helpful if you can feed your baby during the casting process, both bottle and breast feeding can be accommodated as this helps distract them and calm them. For an older child, their favourite toy can also be a useful distraction.
How do I care for my baby in the plaster?
When the plaster cast is first applied, it will take 24 hours for the plaster to dry fully, so you may find clothes and bedclothes get a little damp. During this time, please take extra care not to disturb the plaster in any way. It is important to follow all of the instructions below carefully, to ensure your baby is happy, safe and the treatment is successful. Any of the staff involved in your baby’s care are happy to answer any queries you have.
Please:
- Check your baby’s toes are pink and warm at every nappy change.
- Check your baby’s skin around the edges of the plaster for any signs of the plaster rubbing, for example redness or soreness.
- Keep the plaster dry – your child is not allowed baths during this time other than immediately prior to attending the appointment where it is due to be removed and changed.
- Change your baby’s nappy frequently to avoid soiling the plaster.
It is important to contact the hospital if
- You cannot see your baby’s toes or you think the plaster may have slipped.
- Your baby’s toes are not pink and warm.
- The plaster becomes loose, cracked or crumbly.
- Your baby is crying more than usual and appears to be in pain.
How many times does the plaster need to be reapplied?
The plaster will be applied between four to six times, meaning up to six weekly appointments. Each cast holds the foot in a new position.
2nd Stage: Tenotomy
Following the plaster casting, most children will need to have a release of the tight achilles tendon to ensure that the foot is flexible. This surgery is called a tenotomy. This is a minor procedure and is usually performed in the clinic under local anaesthetic. However, your paediatric orthopaedic surgeon may feel it is more appropriate for the procedure to be performed under general anaesthetic and will discuss these options with you at one of your casting appointments. A further plaster cast is then applied for three weeks allowing for the wound to heal. A final cast change may be included in this healing period depending on the result immediately after the procedure.




Final Stage: Boots and Bar
At this final stage, your baby’s foot or feet will be fully corrected, but to ensure this correction is maintained, your child now be fitted with the boots and bar.
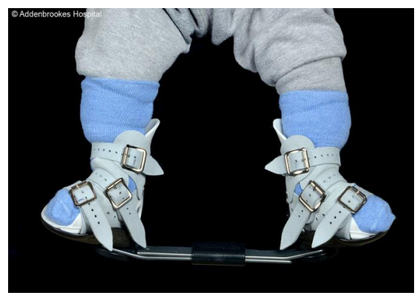

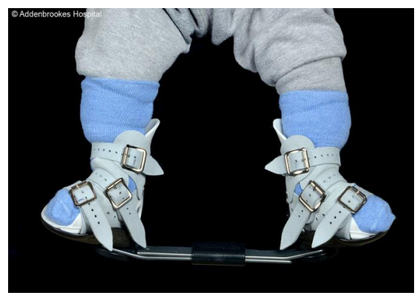

The boots and bar are worn for three months full time (23 out of 24 hours a day), and then are used overnight (10 to 12 hours) on a nightly basis only until your child is five years old. During the day, your child can walk barefoot or wear well-fitting shoes. Once established in their boots and bars, you will still be required to come for regular follow-up appointments, but these will be less frequent, usually between three and six months.
The casting phase is much shorter than the long-term bracing phase and whilst the results are encouraging, it is not a quick fix. It is extremely important that the boots and bar stage is adhered to fully; otherwise there is a significant risk that your child’s foot position will deteriorate to its original starting position. (Please see separate leaflet explaining the boots and bar stage in more details).
Your child is at high risk of the clubfoot returning and further corrective surgery if the treatment prescribed is not strictly adhered to.
Useful contacts:
- The paediatric orthopaedic team secretary: Tel: 01223 216101
- Email the paediatric orthopaedic physiotherapists
- The paediatric orthopaedic specialist nurse: Tel: 01223 254996 or 01223 245151 Bleep 159126
- The plaster room Tel: 01223 217772
- STEPS: the leading charity for children with lower limb abnormalities (opens in a new tab)
- Ponseti group (International) (opens in a new tab)
If you have any problems outside normal working hours, please take your child to your local Emergency Department and contact one of the Addenbrooke’s team as soon as possible on the next working day.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

