Introduction
This information leaflet aims to help you and your family understand more about radiotherapy to treat oligometastatic cancer within the spine, using a technique called stereotactic ablative radiotherapy (SABR). It explains how the treatment is planned and delivered and provides advice to help you look after yourself during and after the radiotherapy. It covers the more common side effects of treatment, but this does not mean that you will necessarily experience them and you may get a side effect not mentioned here. If you have any questions or concerns about the information given to you, or any other aspect of your treatment, please speak to a member of the team.
What is meant by oligometastatic cancer?
This means that the cancer has spread from its original location (metastasised), but is only visible in a limited number of sites on the body scans.
What is stereotactic radiotherapy?
Radiotherapy is the use of high energy x-rays (radiation) to treat cancer. It damages tumour cells to stop them from growing or causes them to die. The purpose of radiotherapy is to destroy the cancer cells while causing as little damage as possible to normal cells.
SABR is an effective way of giving focused radiotherapy, increasing the chance of controlling the tumour whilst sparing normal tissues. It does this by using:
- Fewer treatment sessions
- Smaller more precise radiation fields
- Higher doses of radiation
Radiotherapy itself is painless and does not make you radioactive. It is perfectly safe for you to be with other people, including children and pregnant women during the course of your treatment.
Planning your treatment
Your case will have been discussed at a specialist multidisciplinary team meeting to ensure that radiotherapy is the best treatment option for you.
You will be contacted to attend a telephone or face-to-face clinic in the hospital with your oncologist or specialist SABR radiographer to discuss your proposed treatment. You will be asked to sign a consent form for radiotherapy treatment at this appointment, or a subsequent visit if other tests or results are needed.
If you require any additional medications to take during radiotherapy, this will be explained (for example, a course of steroid tablets (dexamethasone), medication to prevent nausea or additional pain relief).
The MRI and radiotherapy CT planning scan
To plan your treatment accurately you will need a radiotherapy planning CT scan, and in some cases an MRI scan. These may be on the same day and taking around two to three hours in total. You may wish to bring your regular medication with you, and something to read. The radiotherapy planning scan will be in the Radiotherapy Department on Level 2 in Outpatients.
For the CT scan you may need to have intravenous contrast (dye) injected to help enhance the scan. If this is required, you will be asked to fill in a questionnaire and have a cannula inserted. This is a tube that is inserted, usually in the back of the hand or forearm, for the delivery of the contrast.

Treatment position
The position in which you lie during your CT planning scan and radiotherapy treatment will depend on which part of your spine is being treated.
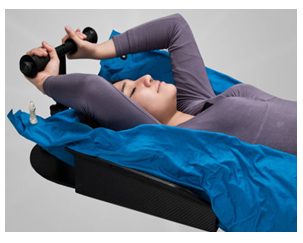
Some patients may be asked to lie with their arms over their head, holding on to a bar. Additional equipment may also be used (shown here in the photograph), which could involve a custom made ‘beanbag’, the air is vacummed out which then forms around you to help support your body. If you have any pain or difficulty keeping your arms above your head, (due to arthritis for example), please discuss this with your clinical oncologist. Taking painkillers 30 minutes to one hour before the planning appointment and treatment can help; which can be prescribed if needed.
Patients receiving radiotherapy to the upper spine, and some patients who are unable to keep their arms above their head, may be treated wearing a mask, as shown in the picture. You will be told if this is required and how you should prepare for it. A mask is individually moulded to your shape and is made from a thermoplastic material. The mask will cover your head, face and shoulders. You can see and breathe through the mask.
It is important that you are comfortable lying in position for up to an hour, as the same position will be used for your radiotherapy treatment. After the scan is finished the radiographers may put some permanent small dots on your skin known as tattoos. These are used to align you in the same position when you come for your radiotherapy treatment. If a mask is required, marks will be drawn on the mask rather than making any permanent skin marks.

The radiotherapy treatment
How are the appointments arranged?
The number of treatments you will receive will depend on various factors, but typically for spinal SABR this is usually three or five treatments. This will be discussed at the time of consent. During the planning stage it may be that the number of treatments you receive changes; if this is the case you will be informed by the oncologist prior to the treatment starting.
We will accommodate your time preferences wherever possible. Please try to be as flexible as possible and give your treatment sessions priority over other general appointments. During the course of treatment, the times may vary each day depending on the number of patients on the unit. Sometimes the Radiotherapy Department can be very busy and your appointment time may be delayed. We will keep you informed of any delays. It is important to make the SABR team aware of any upcoming holiday or other unavailability that could interfere with your proposed treatment schedule.
What happens during my treatment?
On your first day of radiotherapy, a member of the team will have a chat with you to discuss the treatment and how to minimize any potential side effects. They will also check that you are happy to go ahead with your treatment. This is a good opportunity to ask any questions that you may have. Please feel free to bring music on your mobile phone or MP3 player; this can be played through our speakers.
The radiotherapy treatment machine is quite large, but it will not actually touch you. Once you are correctly positioned on the treatment couch, the radiographers will leave the room to switch the machine on. You will be alone in the room during treatment but the radiographers will be watching you on monitors. They can also speak to you via an intercom. If you need help, raise your arm. The machine can be switched off and the radiographers can return to the room to assist you.

Scans will be taken on the treatment machine after, and occasionally during, treatments to check your position; adjustments are made if necessary. The treatment is then delivered. The machines make a buzzing sound when giving the radiotherapy, but it is completely painless. There may be pauses during the procedure when the radiographers are reviewing your images or setting up the treatment. A radiographer may also come back into the room part way through your treatment. Please ensure that you remain, and in the treatment position, until the radiographers inform you that the procedure has finished.
What do I do if I feel unwell?
It is important that you attend each appointment. If you manage to come for your radiotherapy but feel unwell, let your radiographers know as soon as you arrive. However, if you suddenly feel unwell and are unable to come for treatment, please see the contact information below and call the most appropriate number. Please call your GP if it is not treatment related.
What are the side effects of treatment?
Side effects can be divided into short-term (acute) effects that happen during or soon after treatment, and long-term effects occurring months or years later. Some side effects are common, whilst others are rare.
The area and amount of treatment given to you will determine which side effects you are likely to experience. Your oncologist will discuss this with you.
Short term effects (during or up to 12 weeks after your treatment)
Back pain
Some patients might experience pain in the part of the spine being treated after stereotactic radiosurgery. It may be necessary to take painkillers such as paracetamol, if you know you can take these, to ease this pain before it settles down.
- You may be given a short course of steroids (dexamethasone) to take during your treatment. The purpose of these steroid tablets is to reduce swelling at the treatment site and thus minimizing the risk of developing acute back pain.
- If you are already on steroids, the dose may be temporarily increased during your treatment. You will be given instructions about what to do after the treatment is completed. Do not stop your steroids after treatment unless you are given specific instructions to do so.
If you experience severe back pain despite taking painkillers and / or steroids:
- Inform your treatment team when you are next in the department
OR
- Call Addenbrooke’s acute 24 hour oncology helpline: 01223 274224
Tiredness
Tiredness is one of the most common side effects of radiotherapy. Listen to your body. You may need to rest and relax more than usual, particularly if you are travelling long distances to the hospital. However, it is good to maintain a level of activity such as gentle walking, if you feel able. Do not be afraid to ask friends and family for help. Ensure you drink enough fluids as this can prevent tiredness from dehydration.
Skin reaction
Radiotherapy will only affect your skin within the treated area. You may notice that the skin here becomes more sensitive, slightly red, warm, itchy or dry. This may appear in the weeks following treatment.
We advise you to:
- Wash daily with a mild soap and warm water and pat dry with a soft towel
- Apply a gentle moisturiser to the treated area up to twice daily e.g. E45® or Diprobase®
- Use a high factor sun screen or avoid sun exposure to the treated area as the skin here will be more sensitive
Loss of appetite and nausea
Your appetite may vary during and after your treatment. Try to eat well and drink about two litres of fluid every day during your treatment and continue to stay hydrated after treatment too. If you are experiencing significant nausea during your treatment, please let us know as anti-sickness tablets can be prescribed. If this occurs after you have finished your treatment please get in touch with your GP or call the Oncology helpline.
Bowel symptoms
If we are treating your lower spine, you may experience some inflammation of your bowel. This can cause cramping, increased flatulence (wind), loose bowel motions and increased frequency of opening your bowels. You may have an urge to open your bowels but without actually passing anything. Drinking plenty of liquid throughout the day will be beneficial in replacing lost fluids. If you have any concerns, please see contacts below.
Difficulty in swallowing
If your oesophagus is close to the area of the spine being treated (upper thoracic or cervical spine), it may become inflamed during and shortly after SABR treatment. You may experience soreness when you swallow or a feeling of heartburn. You may need to adopt a softer diet temporarily. Cool drinks and ice cream may help. It is advisable to avoid spicy, scratchy or stodgy foods, hot drinks, and strong alcoholic drinks. Soluble paracetamol may help if swallowing is particularly uncomfortable. It may be up to two to three weeks after finishing treatment before this symptom starts to improve.
If you experience severe lack of appetite and pain when swallowing despite taking painkillers:
- Inform your treatment team when you are in the department
OR
- Call Addenbrooke’s acute 24 hour oncology helpline: 01223 274224
Shortness of breath and / or raised temperature
Occasionally, the radiotherapy causes inflammation in the lung tissue. This inflammation or ‘pneumonitis’ can cause symptoms of increased shortness of breath, wheeze, fever or cough. This may occur a few weeks after the treatment has finished. It can often be mistaken for a chest infection but it is not helped by antibiotics. Pneumonitis is rare and is less common in stereotactic radiotherapy compared with conventional radiotherapy. However, if you experience these symptoms, please contact your oncology team, as we may need to review you in clinic sooner than planned. If pneumonitis is suspected, your oncologist may give you steroid tablets to help your symptoms and reduce the inflammation.
Longer term side effects (after around three months)
Your doctor will discuss any potential long-term side effects of SABR to the spine that are relevant to you and the risk of these happening when you consent to treatment. Serious long-term side effects are rare and are dependent on the treatment and location of your disease, but these may include the following.
Back pain, vertebrae and rib fractures
Spinal SABR can weaken the bones in your back (vertebra). If a vertebra is weakened by spinal SABR, it can fracture (break) or collapse. This is called a vertebral compression fracture, which can be very painful. It may be necessary to take painkillers to control the pain. Sometimes the pain caused by vertebral compression fracture may subside after approximately eight weeks. Other patients may need to take painkillers permanently to control the pain. If the pain is severe, a small number of patients may need an operation to help ease the pain.
If the tumour is close to the ribs, there is a chance that the radiotherapy may weaken the ribs and cause them to break. Not all rib fractures are painful, but some patients need to take painkillers for a long period of time if the pain is significant.
Damage to the spinal cord or cauda equina
Spinal SABR can damage the nerves in the spinal cord or the cauda equina (the ‘tail’ of the spinal cord). We take great care when planning and delivering your treatment to minimize this risk. The risk is very small (affecting fewer than 10 people for every 1000 treated) but it would be very serious if it were to happen. Symptoms depend on which part of the spinal cord and which nerves are damaged. Symptoms can include limb weakness, difficulty walking, numbness or loss of bladder and bowel control.
Damage to the oesophagus or bowel
Spinal SABR can damage the oesophagus (gullet) or bowel. The risk is small but it could be serious if it were to happen. Possible symptoms of damage to the bowel include a permanent change in bowel habit, bleeding from the bowel or diarrhoea. Please inform your GP or oncology team.
Other rare, but potentially serious or life-threatening complications include, a stricture (permanent narrowing) of the oesophagus or bowel, perforation (hole) in the oesophagus or bowel or severe bleeding from the oesophagus or bowel. In rare cases, corrective surgery may be needed to treat any serious damage to the bowel or oesophagus.
Damage to the trachea
Spinal SABR can damage the trachea (windpipe) or the main airways (air tubes) into each lung. This can cause a cough or chest infections. It is extremely unlikely that treatment will cause a hole to develop in the trachea.
Lung scarring
Spinal SABR could cause permanent scarring to a small area of the lung. This could cause you to develop a persistent cough and / or you may find you are more out of breath than usual. If you experience any changes to your lung function (cough / breathing), please contact your GP or oncology team.
Psychological effects
This information sheet deals mainly with the physical and practical aspects of your radiotherapy treatment, but the emotional wellbeing of you and your family is just as important. Having treatment can be deeply distressing for some patients. It is not unusual to feel overwhelmed by different thoughts and feelings following a cancer diagnosis. It is important to look after yourself during and after treatment. Advice and support is always available if you are finding it difficult to cope. There are many resources available for patients, their families, and carers to cope with the emotional impact of cancer. Ask one of the treatment team or contact the Macmillan information pod, Maggie’s Centre or the Cambridge Cancer Help Centre for more information.
After treatment ends
Radiotherapy can continue to have a beneficial effect on the tumour for some weeks after the completion of treatment. The side effects from radiotherapy generally persist or worsen slightly for seven to ten days before gradually subsiding over the next two to four weeks.
Follow up appointment
You will receive an appointment to have a follow up with your SABR oncologist about six weeks after treatment has finished. This may be by telephone or at the hospital. If you have not received a notification of that appointment five weeks after the end of your treatment, please telephone the radiotherapy reception and ask to speak to your oncology consultant’s secretary. If you have any concerns or experience any of the above side effects that are not relieved by the advice given, please call the Addenbrooke’s oncology helpline or the SABR specialist radiographer.
Repeat prescriptions
If you need repeat prescriptions of any medication prescribed during your treatment to help with the side effects, these should be available from your GP.
Ongoing follow-up
After your six week follow-up with the SABR team, you will be referred to your original oncology team, with all information being passed onto them as well as your GP.
We do not tend to scan immediately at the end of treatment to see if the radiotherapy has worked. This is because radiotherapy continues to have a beneficial effect on the tumour for some weeks afterwards, and the tumour may take time to reduce in size. Radiotherapy also causes inflammation in the surrounding tissue meaning that x-rays and scans at that time are not so helpful.
If you are worried or notice any new symptoms between appointments, you must let your oncology key worker / specialist nurse or GP know as soon as possible.
Contacts
If you have any worries or questions about any aspect of your treatment, please do not hesitate to contact one of the team.
Specialist SRS / SABR radiographer
Telephone: 01223 536329
Radiotherapy reception
Telephone: 01223 216634
Oncology reception
Telephone: 01223 216551 / 01223 216552
Addenbrooke’s acute 24 hour oncology helpline
Telephone: 01223 274224

Cambridge Cancer Help Centre

Maggie's
Telephone: 01123 249220
Email Maggie's

Macmillan Cancer Support
Telephone: 01123 274801
Email Macmillan Cancer Support
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

