Who is the leaflet for?
This leaflet is for patients who have attended an initial clinical psychology appointment in the pain service.
What is its aim?
The leaflet explains to you and your family what may be involved in a psychology treatment based on a cognitive behavioural understanding of chronic pain. The leaflet will also help you to understand what you may expect to gain from individual clinical psychology sessions.
How could this information help?
This information will help you to decide whether to take up a series of sessions with a clinical psychologist. It will encourage you to think about whether psychology sessions might be helpful at this point in time. At the initial appointment, we talked with you to form a shared understanding of the range of issues you cope with. At your follow up appointment, there will be an opportunity for you to raise any questions and for us to come up with an agreed plan.
What is a cognitive behavioural approach to chronic pain?
A cognitive behavioural approach to chronic pain involves you meeting with a psychologist to think about how chronic pain affects your life. There will be an opportunity to think about goals to work towards in psychology sessions. It is a talking therapy and you take an active role. In this process you may look at how you think about yourself, the world and other people. You may think about links between what you do, your thoughts, and your feelings. You might think about healthy habits, like eating well and getting enough sleep, and how pain can affect your relationships with other people. The cognitive behavioural approach teaches you ways to challenge unhelpful thinking patterns and how these strategies can help improve feelings and behaviours.
Patients who have attended an initial psychology appointment have highlighted areas of difficulty, such as:
- How you think can affect how you adapt to your chronic pain: Patients often report avoiding activities due to fear of pain, resulting over time in further loss of physical function. They find themselves focusing on identifying a cause of pain, or a cure.
- Your mood can be affected by your pain: Patients experiencing chronic pain often suffer symptoms of anxiety, low mood and / or frustration. For example, some patients have beliefs about how they ought to cope with their pain. When they are not able to cope with their pain, they may believe that they are failing and, over time, they may lose confidence and become de-motivated.
- Your social and family relationships can be affected by: how you think about your condition; messages you received from family members coping with illness when you were growing up; and how you currently communicate with others about your pain condition. Anxiety around talking about pain may in turn affect your pain condition and cause further difficulties.
How could a cognitive behavioural approach to managing pain help me?
The cognitive behavioural approach to managing chronic pain focuses on your current ways of coping. It can be useful to look at how your pain can be affected by things that you have experienced in the past. However, we also think about your current coping strategies that are helpful for managing chronic pain.
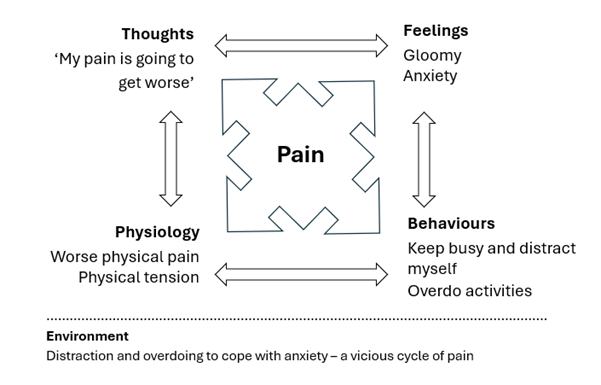
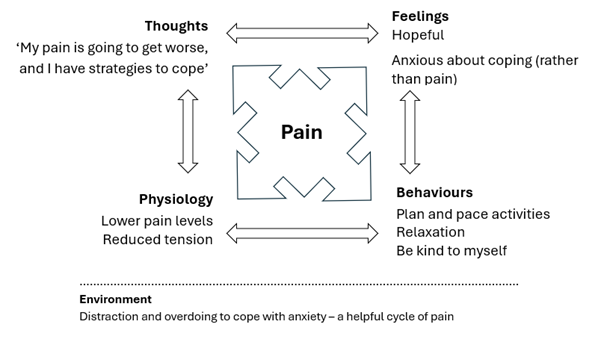
The psychological approach helps to normalise the distress that can be difficult to talk about in everyday life. By thinking about current difficulties that you are experiencing, you can gain an increased awareness of how behaviour patterns can affect your pain levels, and identify alternative responses. Figure 1 gives an example of how a pattern of thoughts and behaviours may make you feel worse, adding to a cycle of chronic pain. Figure 2 gives an example of a more helpful cycle.
The approach will also help you to see how unhelpful cycles of pain develop. You can try out different ways of responding to pain by thinking about the skills you already use for pain management. You will also learn new skills to practise and you may find you can make more informed choices in how you respond to pain. In turn, you may gain an increased sense of control in your life and begin to feel better.
Example situation: distraction as a way of coping
What does treatment involve?
Following the initial conversation, usually a review appointment will be offered to cover any questions, to agree the contents of an assessment letter and to come up with a plan. For many patients, the focus will be towards valued activities and achieving realistic goals. You may find that directed self-help information if this is all that you require. We will consider whether a cognitive behavioural approach is appropriate for you. If this approach is appropriate, and you are able to commit the time, we will work with you to develop a treatment plan. If a cognitive behavioural approach is not appropriate, we may discuss a referral to other specialist pain teams or services.
A typical treatment plan involves a series of six to twelve fifty-minute appointments carried out with the clinical psychologist. Where possible this is on a weekly or fortnightly basis. As part of planning treatment, we work with you to agree personalised goals. The treatment process involves working together to identify factors that help to maintain ongoing problems with persistent pain that it may be realistic to work on. This therapeutic approach usually involves setting homework to complete, which means trying out new strategies for coping in everyday life. We review your progress with you at each session.
There are set review points to consider how you are finding the approach and how you feel about the progress you have made in the sessions. At these review points, we will discuss whether further sessions are appropriate. If not, we will discuss options for discharge from pain clinic psychology.
There is usually an emphasis on maintaining beneficial change, preventing relapse, and working towards discharge.
Benefits
Chronic pain can involve interactions of biological factors, existing habits and behaviours, thoughts, feelings, social relationships and cultural factors. The clinic takes this perspective on a patient’s chronic pain to help them understand and self-manage chronic pain as best they can. The aim is not to cure pain but to help patients resume everyday activities, feel better, and make gains in what they can do.
There is substantial research literature to suggest the benefits of a multidimensional approach to pain management, informed by a cognitive behavioural understanding of the problem. Cognitive behavioural therapy (CBT) was recommended by NICE in 2021. The National Institute for Health and Clinical Excellence produces guidance to promote good quality healthcare. CBT is a treatment of choice for people with chronic pain and is also recommended by the British Pain Society
Risks
There are no known frequently occurring risks associated with self-management and cognitive behavioural approaches to chronic pain. The clinic will aim to meet the recommended benchmarks and be up to date on sufficient quality practice-based evidence. The clinic follows a standard assessment schedule to identify problems and as an aid to decisions on suitability.
There is a risk that you may feel worse at stages during the intervention. One of the reasons for this is because we often spend more time thinking and talking about difficult experiences, which often brings up emotions and thoughts that you may not have experienced in some time. We will work with you in sessions to plan for ways of coping with distress.
Some patients decide to postpone sessions until they feel they can commit, in which case, brief input can be discussed with the patient that is individually tailored to their needs.
Alternatives
Should you require discussion of this or other options, you can contact one of the clinic nurses, the clinical psychologist, or your general practitioner. You may wish to consider another option for accessing clinical psychology or counselling input via your general practitioner.
Contacts / Further information
- The leading mental health charity in the UK is Mind (opens in a new tab):
Mind, 15-19 Broadway, London, E15 4BO, United Kingdom.
Mind information line telephone number: 0845 766 0163
- More information on cognitive behavioural therapy is available on the British Association for Behavioural & Cognitive Psychotherapies website (opens in a new tab), the lead organisation for CBT in the UK.
- The professional body for psychologists in the UK is the British Psychological Society (opens in a new tab) (BPS).
British Psychological Society, St Andrews House, 48 Princess Road East, Leicester, LE1 7DR, United Kingdom.
BPS telephone number: 0116 254 9568
References / Sources of evidence
https://livewellwithpain.co.uk/ (opens in a new tab)
A recommended book on self-management of chronic pain is: Manage your pain. Practical and positive ways of adapting to chronic pain. Michael Nicholas and Alan Molloy. 2003. Souvenir Press.
2021 NICE guidelines: https://www.nice.org.uk/guidance/ng193 (opens in a new tab)
Attendance at appointments
We look forward to seeing you at all your psychology appointments. If under exceptional circumstances you cannot attend an appointment, please contact the administrator as soon as possible, so that we may re-schedule your appointment and offer your cancelled slot to another patient.
Due to service demand and Trust policy, we are required to discharge you from the psychology service if you cancel two consecutive appointments or do not attend a scheduled appointment. We will write to you to discharge you from psychology and send a copy to your GP. We acknowledge on occasion there are unexpected circumstances so please do contact us if this occurs. If your GP writes to the service within six months of discharge you can be returned to the psychology waiting list.
Privacy and Dignity
If you have any concerns at any stage, please speak to the sister or clinical nurse specialist at the pain clinic.
The department of pain medicine is compliant with Trust policies for patient confidentiality. Sessions are confidential unless it is thought by the therapist that your own or another person’s safety is at risk or if you wish members of the pain team to share your information. Clinical notes from sessions are kept separate from your medical notes. Your assessment letter is discussed with you before it is sent to your GP.
All therapists receive supervision of their work with clients to ensure patient safety, this is completed anonymously and is strictly confidential. We continue to work on ways to improve the pain service. We would welcome your comments on your experience of clinical psychology as part of the pain service. We would also welcome your feedback on this leaflet. Should you like to comment please write to:
Pain Clinic Administrator, Department of Pain Medicine, Box 215, Addenbrooke’s Hospital, Hills Road, Cambridge, CB2 0QQ
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

