Who this leaflet is for and what is its aim
This leaflet is for patients who have been diagnosed with abdominal aortic aneurysm (AAA) and have been recommended to have surgery.
This leaflet aims to explain the procedure and its risks.
Background Information
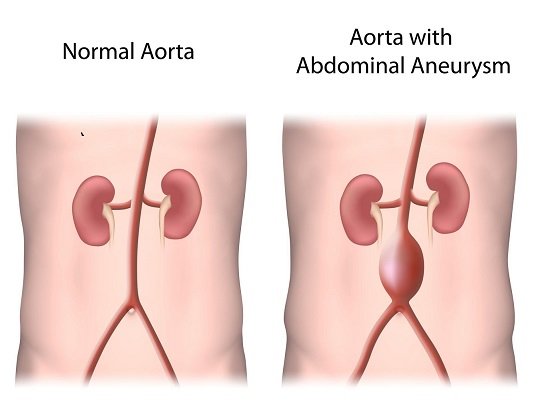
An arterial aneurysm is an abnormal dilatation (ballooning) of an artery caused by a weakness in the wall of the artery. Generally, an artery is called aneurysmal when it increases to more than 1.5x its normal size.
Any artery in the body can develop an aneurysm but some arteries are more commonly affected than others. The aorta, which is the main artery in the abdomen, is the most commonly affected. Other arteries affected are the iliac arteries (in the pelvis), the femoral arteries (in the thigh), and the popliteal arteries (behind the knee).
An abdominal aortic aneurysm (AAA) is an abnormal dilatation of the aorta, which is the main artery in the body and carries blood away from the heart. The other arteries in the body are supplied by the aorta, for example those that supply blood to the head, limbs and body organs. The part of the aorta that lies below the kidney arteries and above the iliac (pelvic arteries) is particularly prone to this problem.
The main risks of aneurysms are either that they burst (leading to life-threatening bleeding) or they block, thus cutting off the blood supply to the areas they support.
Aneurysms are more common in people aged over 60 years. They are also more common in males than female and in those who smoke or have smoked in the past. Aneurysms can also run in families.
Diagnosis of AAA
The majority of AAAs cause no symptoms and are discovered by chance. A routine examination by a doctor or an ultrasound scan performed for some other reason may pick up the presence of an aneurysm. Alternatively, some patients notice an abnormal pulsation in their abdomen (tummy). Routine screening for aneurysms has been established for men aged 65 throughout the UK.
Investigation of AAA
The majority of AAA can be diagnosed with a simple ultrasound scan, which also provides an accurate measurement of its size. The risk of rupture (bursting) of AAA is related to its size: AAA bigger than 5.5 cm in diameter for men or 5.0cm in diameter for women are at a higher risk of rupture and require surgical repair to avoid this.
Smaller aneurysms are monitored with ultrasound scans every three to twelve months depending on size, and surgery is only considered if they increase in size rapidly, or start to cause pain or other symptoms.
When an aneurysm requires surgical repair, other investigations are arranged including a CT body scan. This provides accurate anatomical information regarding the aneurysm so the operation can be planned in more detail. The CT is also used to decide if a stent is possible alternative for repair of the AAA.
Other investigations to measure the function of the heart, lungs and kidneys might also be arranged, because this surgery tends to put an extra strain on these organs.
Possible Blood transfusion
Open AAA surgery is a major vascular operation and blood loss is expected and anticipated. A special suction machine called a Cell Saver is used to suction up blood from the operative field, it is then processed and immediately returned to you during the operation. This significantly reduces the likelihood of you requiring a blood transfusion of donated blood. However, if you lose a considerable amount of blood you may also require a blood transfusion.
The blood transfusion can involve giving you other blood components such as plasma and platelets which are necessary for blood clotting.
Your doctor will only give you a transfusion of blood or blood components during surgery, or recommend for you to have a transfusion after surgery, if you need it.
Compared to other everyday risks the likelihood of getting a serious side effect from a transfusion of blood or blood component is very low. Your doctor can explain to you the benefits and risks from a blood transfusion. Your doctor can also give you information about whether there are suitable alternatives to blood transfusion for your treatment. There is a patient information leaflet for blood transfusion available for you to read. If you do not wish to receive a blood transfusion should it be required, please discuss this with your surgeon.
During the procedure
At the start of the surgery, we make an incision (cut) in the abdomen. Through this incision we dissect (make visible) the normal aorta above and below the aneurysm and then stop the blood flow through the aneurysm by applying vascular clamps.
We then replace the aneurysmal (damaged) section of the aorta by sewing in a tube of special artificial vascular graft material. The blood flow through the aorta can then be restored and the incision closed. Commonly, patients recover from aneurysm surgery in the theatre recovery area or intensive therapy unit (ITU).
After the procedure
Once your surgery is completed you will usually be transferred to the recovery ward where you will be looked after by specially trained nurses, under the direction of your anaesthetist. The nurses will monitor you closely until the effects of any general anaesthetic have adequately worn off and you are conscious. They will monitor your heart rate, blood pressure and oxygen levels too.
You may be given oxygen via a facemask, fluids via your drip and appropriate pain relief until you are comfortable enough to return to your ward.
At this time, there will also be a urinary catheter inserted into your bladder, which allows your urine to drain into a bag. This is a temporary measure to help monitor your fluid requirements and prevent urine becoming retained. Once you are mobile enough to use the toilet, this can be removed. This is usually 3-5 days after the operation.
After open AAA surgery, most patients are transferred to the intensive care unit (ICU/ITU), high dependency unit (HDU), intermediate dependency area (IDA) or fast track/overnight intensive recovery (OIR).
These are areas where you will be monitored much more closely because of the nature of your operation or because of certain pre-existing health problems that you may have.
Risks
Risks
Open repair of AAA is a major surgical procedure. Over the last two decades major improvements have been made to make the operation as safe as possible and rates of major complications are at an all time low.
Results from surgery are published at Vascular Services Quality Improvement Programme (opens in a new tab) and you can look up the outcomes for CUH and other vascular centres in the country. Despite these recent advances a small number of patients do not survive the operation.
In 2023, the National in-hospital mortality following open AAA repair was 3.0%. At CUH, the mortality is consistently lower than 1%.
As the aorta is such an important blood vessel other serious complications can occur. Rare, but significant complications include:
· Damaged blood supply to the legs requiring further surgery. In rare circumstances a major amputation of the leg is required.
· Damaged blood supply to the kidneys and occasional need for dialysis to support the kidneys.
· Damaged blood supply to the spinal cord and neurological damage to the lower limbs (paraplegia). This is rare and occurs in 1/500 cases.
· Damaged blood supply to the intestines. Occasionally further operations are required for this and can require formation of a stoma on the abdominal wall. This occurs in approximately 1/30 patients.
· Occasionally there are bleeding complications after the operation requiring a return to the operating theatre.
· Clamping the aorta prior to repair can put some strain on the heart and this sometimes leads to a myocardial infarction (heart attack).
Other complications that can occur include infections (in the lungs, wound, abdomen or urinary system) and something called ‘ileus’. This is where the bowels take a while to start working after the procedure. In approximately 1/10 patients this can be prolonged (>3-4 days) and require feeding through a vein.
Once you leave hospital, open repair of AAA is for the most part a durable operation and further surveillance is not required. There are, however, some longer term potential complications. These include incisional hernia and intestinal obstruction (caused by scar tissue). Occasionally further surgery is required to address these. Approximately 10-20% of men experience erectile dysfunction post-operatively.
Rarely the graft that is implanted to your aorta can become infected. This is rare but can be a very serious complication if it does occur and further surgery is sometimes required.
Alternatives
Monitoring only
Although intervention is considered when the AAA reaches 5.5cm in men and 5.0cm in women, it is not appropriate for all patients. For example, there may be patients that are very high risk for surgical intervention because of pre-existent illnesses.
In this group continued surveillance and a higher intervention threshold may be appropriate. Sometimes no surgery is the best option.
Information and support
We may give you additional patient information before or after the procedure, for example, leaflets that explain what to do after the procedure and what problems to look out for. If you have any questions or anxieties, please feel free to ask a member of staff or our Vascular Specialist Nurses on 01223 348526 or Email
Further information is available from The Vascular Society Website: The Vascular Society (opens in a new tab)
Medication
Please bring with you all of your medications and its packaging (including inhalers, injections, creams, eye drops, patches, insulin and herbal remedies), a current repeat prescription from your GP, any cards about your treatment and any information that you have been given relevant to your care in hospital, such as x-rays or test results.
Please tell the ward staff about all of the medicines you use. Take your medications as normal on the day of the procedure unless you have been specifically told not to take a drug or drugs before or on the day by a member of your medical team. Do not take any medications used to treat diabetes.
Pharmacists visit the wards regularly and can help with any medicine queries.
My Chart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device
More information is available on our website: MyChart
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

