Introduction
This leaflet will provide you and your family or carers with some information about osteoarthritis (OA) to help you understand your condition as well as a summary of self-management techniques we have discussed today. These techniques cannot cure your OA but can help to reduce the pain you experience and slow the deterioration at your joints. This will help you to continue with your usual daily activities.
What is osteoarthritis
Osteoarthritis is a degenerative condition, which means it can worsen over time. It affects around 10 million people in the UK. It is a non-inflammatory type of arthritis and is often referred to as wear-and-tear, as the cartilage between the joints wears down. This reduction in the cartilage causes friction between the bones and can cause pain, swelling and reduced movement of the joint.
Pacing
One technique that we discuss is ‘Pacing’. Your daily tasks are broken down into smaller or shorter activities to make to make them more manageable. People who suffer from osteoarthritis often describe that their pain is increased with certain activities or that they have good days and bad days. Pacing is a way to be able to do your everyday and meaningful activities without increasing your symptoms.
Ways to pace an activity can include taking regular breaks, changing your body positions regularly, gradually increasing the time you spend doing a particular activity over time and stopping an activity before it becomes painful.
Joint protection
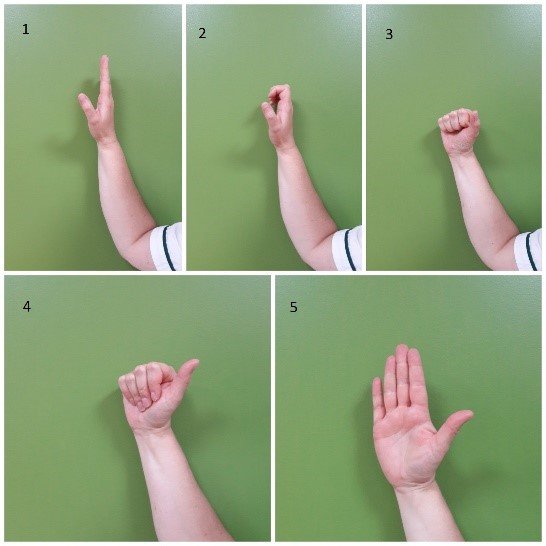
We also discuss joint protection. The main principles of joint protection are
1) Use bigger joints- for example carry your shopping bag on your forearm, in a backpack or use a trolley. Bigger joints in our bodies, such as arms, legs or back, are designed to take more of a load.
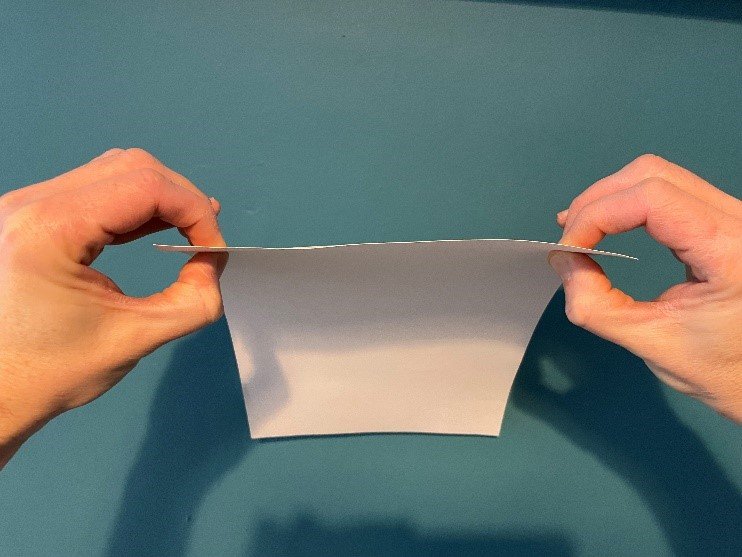
2) Use more joints- for example carry a plate with both hands or open a cupboard with all the fingers on your hand. This will spread the load across the joints reducing the force through the joints affected by OA.
3) Use gadgets to assist you. Using gadgets, for example, for opening jars or tins, or using an ergonomic knife. These will help to spread the load on a joint or change the way the joint moves. This reduces the force that you need to apply and therefore make the activity less painful.
Pacing and joint protection principles both involve developing new lifestyle habits. As we get older changing habits can take time so you should start with small changes and build on this over time. Make a plan, write it down, and put it where you will see it easily, maybe on your fridge or wardrobe door can be helpful. Use your plan to help you to measure your day or week’s progress. Measuring your progress can help to keep you motivated. If your fall back into old habits, stop and reflect on this but do not give yourself a hard time.
Equipment/gadgets for the kitchen
- Jar key – releasing air from the jar to make it easier to open
- J-hook – to use for ring pull on tins
- Wire meshing cooking basket – for boiling veg/pasta, by placing inside pan
- Dycem – rubber mats and domes for opening jars/bottles
- Good grip peelers and other utensils
- Loop scissors
- Plug pulls
- Ergonomic knives
Insulation piping on handles of tools or cutlery can be useful to try first to see if a thicker handle will be of benefit. The insulation piping is also very portable to keep in your bag or coat pocket to carry with you.
Problem solving
Normal everyday activities can be difficult if you have OA. Pain, reduced range of movement at affected joints, fatigue and reduced strength all have an effect on your day-to-day activities. Problem solving can be used to help with these issues. You do not necessarily need to change the whole task as sometimes a small change will help.
How to problem solve:
- Identify the activity that is causing a problem
- Decide if it is the whole task that is difficult or parts of it
- Consider various possible options/techniques to address the problem and write them down
- Select one option to try
- Try the option and reflect if it worked or helped
- If it helped, continue to practice the new way of doing activities until it becomes habit. If it did not help, select another option to try and, again see if it helped
Oedema management
Oedema (also known as swelling) is when fluid goes to a particular point of the body to help it repair, usually after an injury or trauma. This is usually normal re-action to an injury or trauma but can limit movement. There are a few things you can do at home to help manage this:
Contrast bathing
- Fill one bowl with cool water from the tap. Fill the other bowl with warm water from the tap. Test the temperature of the warm water with your uninjured hand first to make sure it is not too hot.
- Put your whole hand in warm water for about one minute, then switch to the cool water for about 30 seconds.
- If your therapist advises you to, move your fingers/thumb when they are under the water.
- Continue switching between the bowls seven times. Repeating the process of warm water for 1 minute then cool water for 30 sec.
If this treatment makes any of your symptoms worse, then stop immediately.
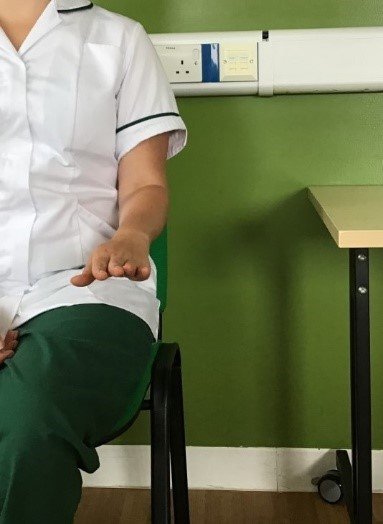
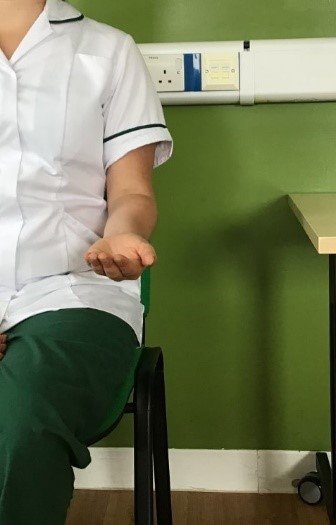
Retrograde massage
Sit comfortably with your elbow resting on the arm of a chair or table with your hand in the air. Apply any kind of moisturising cream to your hand or finger and stroke from the tip of the finger down into the hand and down to the wrist. Always work in a downwards motion, starting from the top and working down the swollen area. The strokes should be long, smooth and firm so that the excess fluid is pushed out of the finger or hand, as far away from the swollen area as possible
Relaxation
Relaxation is the feeling of calm. People with chronic pain can feel muscle tension as a response to their pain. This muscle tension becomes part of their pain and may contribute greatly to it Getting rid of, or reducing, that muscle tension can help to reduce the pain. Day to day, normal life can, at times, be very stressful for a number of reasons, some of these stresses maybe short term e.g. moving house but others can last longer such as living with a long-term condition, relationship issues or problems at work. Stress can add to our pain levels. Regular relaxation can help with these issues/stress factors and also can improve sleep.
Relaxation skills take a long time to learn. If possible, these techniques should be done daily. Do not wait until you have a day when the pain is very severe to try relaxation for the first time, because it probably will not work. Practicing these techniques should be done on the good days, when your pain level is not so high, so that hopefully your bad pain days may be less frequent. Then, when you have bad days, you can lessen the amount of discomfort you have by using the techniques.
Further information
Versus Arthritis (opens in a new tab) - this website/organisation provides further information on your condition. It has further information on how to gain advice and support, including some groups or social events that may be in your area. They have a helpline and can help to signpost you to other resources that may be of relevance.
MyChart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/