Omnipod Handbook (Open Loop)
This booklet has been written to provide you, your family and/or carers, with the information you need when using an Omnipod DASH/ Omnipod 5 insulin pump.
Please refer to the additional closed loop supplement if using the Omnipod 5 with continuous glucose monitoring (CGM) in SmartAdjust.
Non-urgent advice: Insulet contact number
Telephone: 0800 011 6132 or +44 20 3887 1709 if calling from abroad
Please note that the pump companies will not give medical advice and can only offer technical support if you are having problems with the pump.
Website: Omnipod
Immediate action required: Urgent Advice
- If you are feeling ill or have an emergency diabetes or pump problem out of hours, contact the Type 1 Emergency Out-of-Hours Service.
- Contact the diabetes educators if you do not have this number
- Or attend your nearest accident and emergency department
Non-urgent advice: Important Information
Insulin pumps provide clever technology to better manage glucose levels, but the basics remain important. These include:
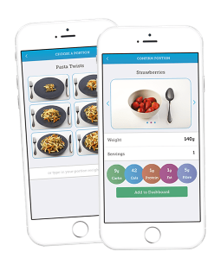
- Accurate carbohydrate counting
- Entering all carbohydrates eaten into the pump (except hypo treatment)
- Timing of the mealtime/snack insulin – a bolus given 10-15 minutes before eating is recommended
- Regular pod changes
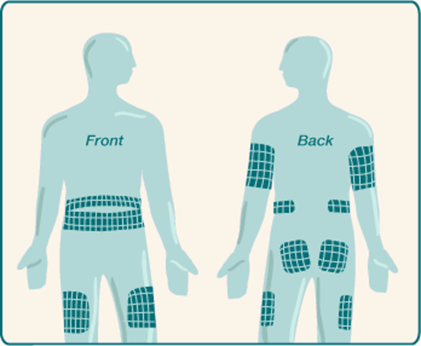
- Rotation of infusion sites
- Optimal hypo treatment
- Adjustments for activity
Non-urgent advice: Recommendations for checking your basal rates:
Recommendations for checking your basal rates:
- We would suggest starting with your overnight basal rates
- We would suggest doing these checks a few times on days that are similar to ensure there is a pattern before you make any changes
- Ideally your glucose level at the start of each check should be between 5 and 10 mmol/L (up to 12 mmol/L can work)
- Choose a day to basal check when you;
- Have not had a hypo of 3.5 mmol/L or below in the past 12 hours
- Have not been significantly more active than normal
- Have not been unwell or are under more stress than usual
- Have not had a significant amount of alcohol in the past 12-24 hours
- Abandon this check if you have a hypo or if your glucose levels go above 12 mmol/L and correct
| Time Frame | What to do | When to check glucose if not wearing a sensor |
|---|---|---|
|
Time Frame
Overnight check |
What to do
Begin review if pre bed glucose is 5-10 mmol/L Eat an evening meal that contains 50g or less carbohydrate that you are confident you will count accurately Do not consume any food or carb- containing drinks for the rest of the evening. Do not exercise |
When to check glucose if not wearing a sensor
3-4 hours after evening meal Bedtime (if not the same time as above) 2-3am On waking |
|
Time Frame
Morning check |
What to do
Begin review if pre-breakfast glucose is between 5-10 mmol/L Skip breakfast Eat no food until lunch |
When to check glucose if not wearing a sensor On waking and every 2 hours until lunch |
|
Time Frame
Afternoon check |
What to do
Begin review if pre-lunch glucose is 5-10 mmol/L Eat a breakfast that contains 50g or less carbohydrate that you are confident you will count accurately Skip lunch No food or carb containing drinks until evening meal |
When to check glucose if not wearing a sensor
3-4 hours after breakfast Then every 2 hours until evening meal |
|
Time Frame
Evening check |
What to do
Begin review if pre-dinner glucose is 5-10 mmol/L Eat a lunch that contains 50g or less carbohydrate that you are confident you will count accurately Do not have an evening meal or carb-containing drinks Eat a late snack if needed |
When to check glucose if not wearing a sensor
3-4 hours after lunch Every 2 hours until your late snack |
Non-urgent advice: Glucose levels
If the glucose levels rise or fall more than 2 mmol/L during the review period this can suggest the basal rates need adjustment.
Adjust the basal rate for the time period 60 – 120 minutes before and up to when the rise or fall in glucose occurs
Adjust the basal rate by 10-20% or by 0.05 or 0.10 units/hr either up or down depending on whether your glucose rose or fell
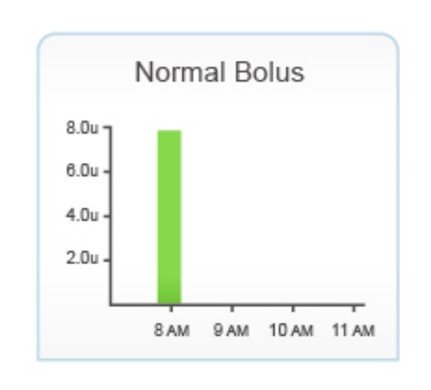
Normal/Standard
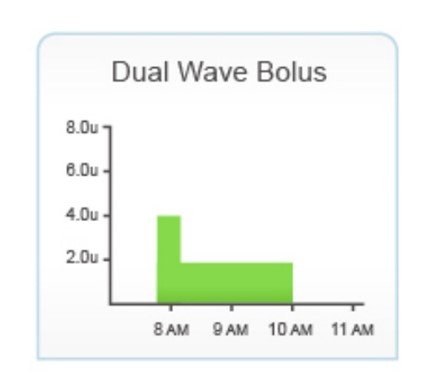
The full amount of insulin is delivered immediately to cover the carbohydrates eaten. Most people start with this delivery until their basal rates and bolus ratios are correct.
| Timing | Target post meal glucose |
|---|---|
| Timing 2 hour post meal glucose | Target post meal glucose Within 2.8 mmol/L of pre-meal glucose |
| Timing 4 hour post meal glucose | Target post meal glucose Within 1.7 mmol/L of pre-meal glucose |
If the glucose level is out of target, review your insulin to carbohydrate ratio:
- If the glucose level rises higher than these levels increase the insulin dose by decreasing the carbohydrate ratio by 10-20% or by 0.5 to 1g
- If the glucose levels drop after a meal then reduce the insulin given by increasing the carbohydrate ratio by 10-20% or 0.5 to 1g
If at any stage during the process your glucose level drops below 4 mmol/L, abandon and have a snack. Repeat the process at another time to confirm the result.
Examples of how to change your ratio following a bolus check…
- Current insulin : carbohydrate ratio = 1unit:15g
Pre-meal glucose = 5.5 mmol/L, 2 hours post meal = 10 mmol/L
Increase the amount of bolus insulin by reducing the carbohydrate part of the ratio by 10-20% to 1unit:14g or 1unit:13g
Repeat the process to check whether the change was appropriate.
- Current insulin : carbohydrate ratio = 1unit:8g
Pre-meal glucose = 6.3 mmol/L, 2 hours post meal = 4.1 mmol/L
Reduce the amount of bolus insulin given by increasing the carbohydrate part of the ratio by 10-20% to 1unit:9g or 1unit:10g
Repeat the process to check whether the change was appropriate.
Note: The lower the carbohydrate ratio, the more insulin the pump will deliver to cover carbs. The higher the carbohydrate ratio the less insulin the pump will deliver to cover carbs.
| Possible cause | Possible solution |
|---|---|
|
Incorrect basal rate |
Possible solution
Check time on handset is correct If you use different basal patterns check you are using the correct one. Too much basal insulin for the activity and a reduced temporary rate basal is needed. Consider checking your basal rate if you notice there is a pattern of when your hypos occur. |
|
Incorrect bolus given |
Possible solution
Check bolus history Check that your carbohydrate counting is accurate Check the timing of bolus for food Consider type of bolus used |
|
Increased activity |
Possible solution
Consider a reduced temporary basal rate for future activity Consider extra carbs for future activity |
|
Hot weather |
Possible solution
Consider a different basal pattern for holidays or summer. Consider a reduced temporary basal rate. |
|
Drinking alcohol |
Possible solution
Consider a temporary basal overnight (up to 10am) if drinking more than 2 units or Consider a carbohydrate bedtime snack Consider reduced bolus at breakfast the next morning. |
|
Incorrect insulin |
Possible solution
Always check the following on a new insulin vial: insulin type, strength, expiry date and how it has been stored. |
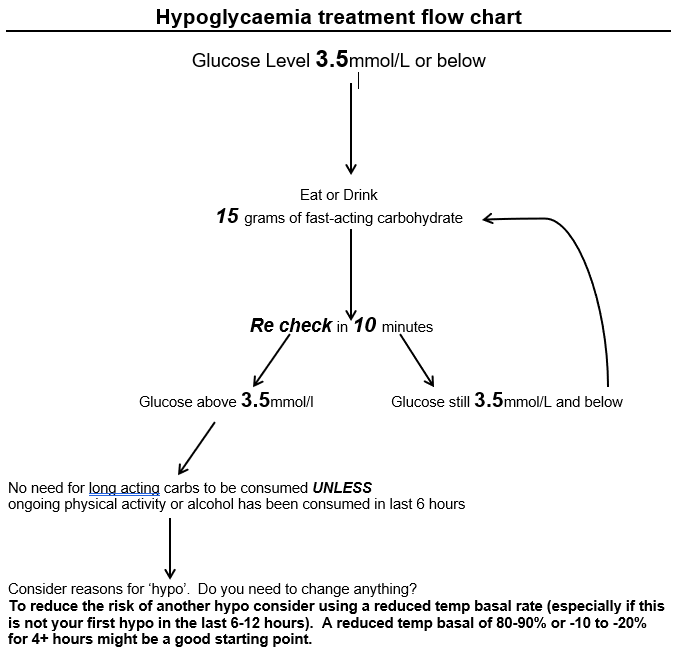
It is important to share this information on correct hypo treatment with close family and friends so that they can assist you, if necessary, to treat a hypo safely.
- Remember to carry quick acting carbohydrate with you at all times for treating hypoglycaemia.
- Please contact your pump educator if you are having frequent, unexplained hypoglycaemia (more than 2-3 per week) or have an episode of severe hypoglycaemia.
How to manage glucose levels which are below target but not hypo
Pre meal/snack
When you enter a glucose level below target before eating your pump will deduct some insulin from the meal bolus to allow your glucose level to rise back into the target range. You may choose to give the bolus at the start rather than 10 minutes before.
If it is a large meal or high in fat it will take longer to digest so you may wish to split the bolus and deliver half at the start of the meal and the remaining half halfway through the meal.
In between meals
Have a small carbohydrate snack to raise your glucose to an appropriate level without covering with insulin.
For example 5g of carbohydrates will raise your glucose level by 1-2 mmol/L, 10g by 2-3 mmol/L.
Urgent advice: Severe hypos
Please call the diabetes out of hours (Mon-Fri 4pm to 11pm and 6am to 9am, weekends and bank holidays 6am to 11pm) emergency number if you (or your relative/carer) require support during or following a severe hypo.
Speak with the diabetes team if you do not have this number.
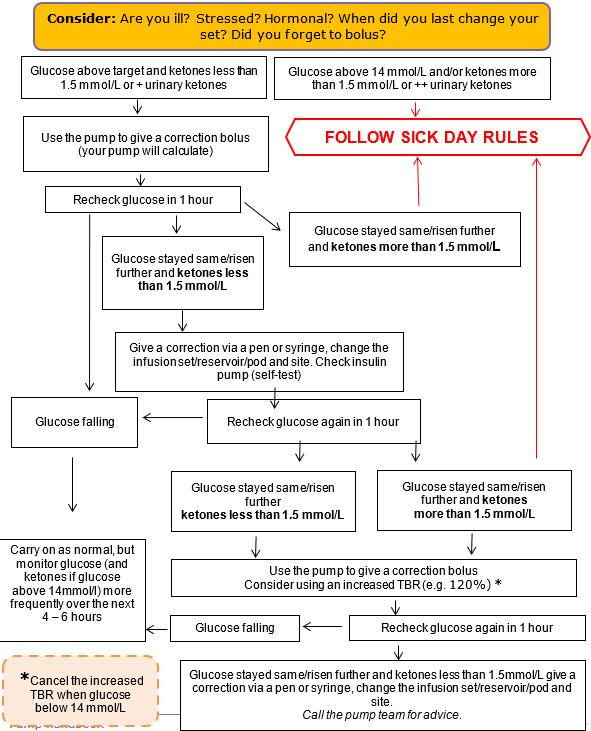
| Possible cause | Possible solution |
|---|---|
| Possible cause Incorrect basal rate |
Possible solution
Check that the time on handset is correct If you use different basal patterns are you using the right one? Consider basal rate review |
| Possible cause Incorrect bolus given |
Possible solution
Check bolus history Check carbohydrate counting accuracy Check timing of bolus for food |
| Possible cause Less active/ more stress/ currently unwell/ menstrual cycle |
Possible solution
Consider using an increased temporary basal rate if the cause is temporary. |
| Possible cause Cold weather/high altitude/dehydration |
Possible solution
Consider a different basal pattern for holidays or winter Consider an increased temporary basal rate if the cause is temporary. Ensure that you drink enough. |
| Possible cause Insulin |
Possible solution
Always check a new insulin vial for damage, the use-by date, strength, correct insulin type. How long has your insulin been out of the fridge? Especially if the weather is hot. |
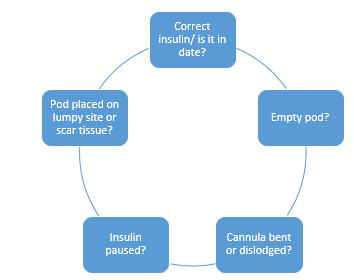
| Possible cause Blocked cannula/ faulty pod |
Possible solution
Are you due a pod change? Did your glucose levels rise with a recent pod placement? Is the infusion site wet? |
Symptoms of hyperglycaemia
- Thirst and dry mouth
- Nausea
- Urgency to urinate frequently
- Vomiting
- Frequent urination especially at night
- Dry or flushed skin
- Impaired vision
- Poor appetite
- Abdominal pains
- Muscular pains
- Difficulty breathing
- Apathy
- Odorous breath
- Fatigue, weakness
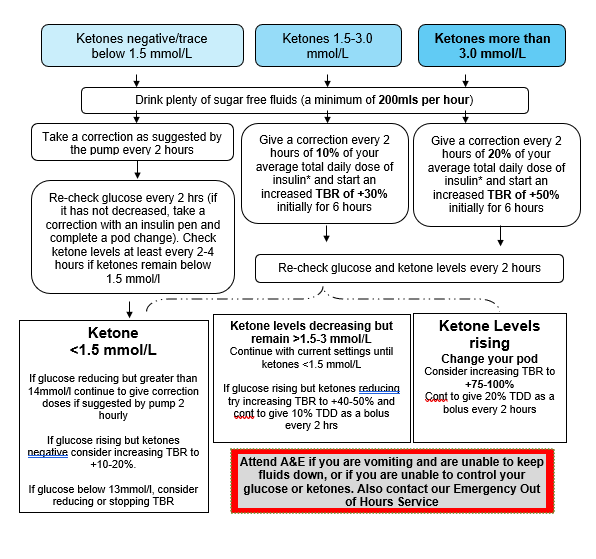
| Total Daily Dose | 10% (additional units) | 20% (additional units) |
|---|---|---|
| Total Daily Dose 20 | 10% (additional units) 2 | 20% (additional units) 4 |
| Total Daily Dose 30 | 10% (additional units) 3 | 20% (additional units) 6 |
| Total Daily Dose 40 | 10% (additional units) 4 | 20% (additional units) 8 |
| Total Daily Dose 50 | 10% (additional units) 5 | 20% (additional units) 10 |
| Total Daily Dose 60 | 10% (additional units) 6 | 20% (additional units) 12 |
| Total Daily Dose 70 | 10% (additional units) 7 | 20% (additional units) 14 |
| Total Daily Dose 80 | 10% (additional units) 8 | 20% (additional units) 16 |
| Total Daily Dose 90 | 10% (additional units) 9 | 20% (additional units) 18 |
| Total Daily Dose 100 | 10% (additional units) 10 | 20% (additional units) 20 |
Your diet when following sick day rules
If you cannot eat normally, try a light diet and eat smaller amounts more frequently e.g. every 2-3 hours. Examples include:
- Bread or toast with soup/egg
- Breakfast cereal
- Crackers/crisp breads/plain biscuits
- Milky puddings or yoghurt
- Milk or fruit juice
This can be supplemented with carbohydrate containing fluids such as milky drinks and fruit juices. Aim to consume a minimum of 30g carbohydrate every 6-8 hours. Cover this carbohydrate with your normal insulin bolus.
If a light diet is not tolerated, take sugary drinks in small amounts more frequently e.g. 10-15g carbohydrate taken every 1-2 hours, for example:
- Normal fizzy drinks (flat – may be tolerated better)
- Sugar-containing drinks e.g. pure fruit juice, cordial, milk
- Lucozade Original
- Ordinary jelly
Medicines
Tablet medications often contain very small amounts of lactose but will not significantly affect glucose levels (usually <2g of lactose per day). Most liquid medications are available in a sugar-free form but some liquids may contain significant amounts of sugar.
A single dose of a sugar containing medication is unlikely to significantly impact glucose levels. Discuss the availability of sugar-free medicines (including over-the-counter medication) with your pharmacist.
| Fast release carbs( shorter sessions/events | Carbs (g) | Slower release carbs (longer sessions/day events | Carbs (g) |
|---|---|---|---|
| Fast release carbs( shorter sessions/events Jelly Babies (4 sweets) | Carbs (g) 20 | Slower release carbs (longer sessions/day events Raisins (30g) | Carbs (g) 22 |
| Fast release carbs( shorter sessions/events Dextrose (4 sweets) | Carbs (g) 12 | Slower release carbs (longer sessions/day events Jaffa cake (each) | Carbs (g) 10 |
| Fast release carbs( shorter sessions/events Isotonic gel (each) | Carbs (g) 22-25 | Slower release carbs (longer sessions/day events Fruit bar (each) | Carbs (g) 15 |
| Fast release carbs( shorter sessions/events Energy sports bar (each) | Carbs (g) 25 | Slower release carbs (longer sessions/day events Cereal bar (each) | Carbs (g) 22 |
| Fast release carbs( shorter sessions/events Energy powder drink (500mls) | Carbs (g) 45-50 | Slower release carbs (longer sessions/day events Malt loaf (1 slice) | Carbs (g) 20 |
| Fast release carbs( shorter sessions/events Gatorade (250ml) | Carbs (g) 15 | Slower release carbs (longer sessions/day events Banana (medium) | Carbs (g) 15-20 |
| Fast release carbs( shorter sessions/events Lucozade Original (100mls) | Carbs (g) 8.4 | Slower release carbs (longer sessions/day events Flapjack (50g) | Carbs (g) 30 |
| Fast release carbs( shorter sessions/events Lucozade Sport (100mls) | Carbs (g) 6.4 | Slower release carbs (longer sessions/day events Fig roll (each) | Carbs (g) 14 |
| Fast release carbs( shorter sessions/events Cola (150ml - mini can) | Carbs (g) 15 | Slower release carbs (longer sessions/day events Oat cake (each) | Carbs (g) 6 |
| Fast release carbs( shorter sessions/events Apple Juice (120mls) | Carbs (g) 15 | Slower release carbs (longer sessions/day events Bread roll (50g) | Carbs (g) 25 |
Taking the pump off
There may be times when you would like to remove your Omnipod temporarily such as swimming, sex and going on holiday.
Insulin pumps should not be disconnected for more than 1–2 hours unless you follow advice in the table below. An Omnipod pump cannot be reapplied if you remove it. You will need to fill and place a new pod.
| Time off the pump for: | What to do: |
|---|---|
|
Time off the pump for:
Up to 90 minutes |
What to do:
Check glucose levels before removing the pod and give a correction if needed using the Omnipod handset. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. When you place the new pod, check your glucose and give a correction if necessary. |
|
Time off the pump for:
Up to 4 hours |
What to do:
Check glucose before removing pod and give a correction if needed using the handset. At 2 hours after removing the pod use your insulin pen to give a bolus of quick acting insulin equivalent to the amount of basal insulin you have missed. For example if your basal rate is 1 unit/hour give a bolus of 2 units. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. When you apply a new pod, check your glucose level and give a correction if necessary. |
|
Time off the pump for:
Up to 12 hours |
What to do:
Check glucose before removing the pod and give a correction if needed using the Omnipod handset. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. Followed by either of the below: Every 2 hours use your insulin pen to give quick acting insulin equal to the missed basal amount or Take a dose of intermediate-acting insulin (Levemir or Humulin I) at the point of removing the pod that is equal to your basal insulin dose for the next 12 hours. If you choose to place a new pod before the 12 hours is up, please run a reduced temporary basal of ↓100% for the remainder of time. Finally: When you place a new pod, check your glucose and give a correction if necessary. |
|
Time off the pump for:
24 hours or longer |
What to do:
Check glucose before removing your pod and give a correction if needed using the pump. If eating use an insulin pen to give a quick acting insulin bolus to cover carbohydrates. Followed by one of the below: Every 2 hours use your insulin pen to give quick acting insulin equal to the missed basal insulin amount. or Take a dose of intermediate-acting insulin (Levemir or Humulin I) at the point of removing the pod that is equal to your basal insulin dose for the next 12 hours. You will need to do this injection twice, approximately 12 hours apart. If you choose to apply a new pod before the 12 hours please run a reduced temporary basal of ↓100% for the remainder of time. or Take a dose of long-acting insulin (Lantus) at the point of removing pod that is equal to your basal insulin dose for the next 24 hours. o If you choose to apply a new pod before the 24 hours please run a reduced temporary basal of ↓100% for the remainder of time. Finally: When you apply a new pod, check your glucose and give a correction if necessary via your Omnipod handset. |
| Time off the pump for: | What to do: |
Please note:
- If you remove your Omnipod for more than 4 hours, close monitoring of glucose levels is recommended.
- We would recommend that you discuss any plans to remove your pod with the pump team beforehand and plan ahead where possible. Disconnecting yourself from the Omnipod puts you at a higher risk of developing high glucose levels and forming ketones /DKA.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/