Introduction
Your baby has been diagnosed with having either oesophageal atresia (OA) and / or trachea-oesophageal fistula (TOF). This information leaflet is designed to guide you through surgery, caring for your baby once they are at home, and throughout childhood.
What is oesophageal atresia (OA) and tracheo-oesophageal fistula (TOF)?
Oesophageal atresia (OA) and tracheo-oesophageal fistula (TOF) are rare conditions of the oesophagus (food pipe) and / or trachea (airway) that affect new-born babies.
Oesophageal atresia (OA)
In oesophageal atresia, the baby is born with a pouch at the top of their oesophagus (food pipe). This means that the oesophagus is not joined to the baby’s stomach, and therefore the baby is unable to swallow any of its saliva or food.
Tracheo-oesophageal fistula (TOF)
In tracheo-oesophageal fistula, the bottom end of the baby’s oesophagus is joined to the trachea (wind pipe). This causes air to pass from the windpipe to the food pipe and stomach.
TOF and OA usually occur together but can, less commonly, occur alone.




What causes OA / TOF?
When a baby is growing in the womb, the oesophagus and trachea develop from one tube. OA and TOF are believed to happen when the oesophagus and trachea fail to separate properly. It is not something that can be prevented, and it is not caused by anything you might have done while you were pregnant.
How are OA / TOF diagnosed?
This condition is rarely diagnosed before birth. It may, however, be suspected when there is more amniotic fluid than usual (polyhydramnios) in the womb, or if an ultrasound has detected other areas of concern.
Usually OA and TOF are found after birth when a baby has either feeding or breathing problems. Your baby might have had problems swallowing their saliva, or seem to be choking on their milk. The midwife or nurse caring for your baby may have tried to pass a tube through your baby’s nose into their stomach (nasogastric tube or NG tube), and found that it was not possible.
Your baby will need an X-ray to confirm the diagnosis.
What happens to my baby after diagnosis?
Once a diagnosis is made, the doctors looking after your baby will make a referral to the paediatric surgery team who will come and meet you and your baby, and explain the next steps.
Sometimes babies can have breathing difficulties and will need a breathing tube and help with their breathing from a ventilator.
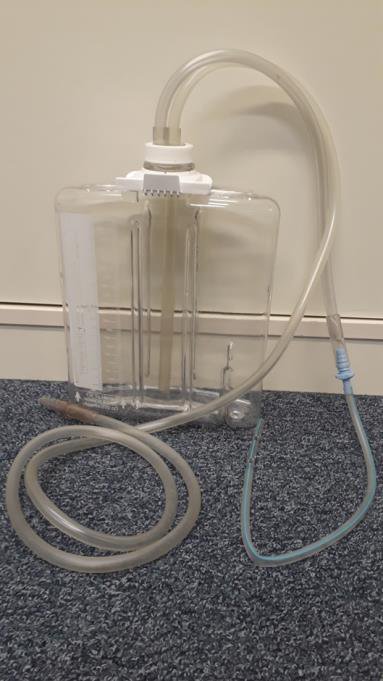
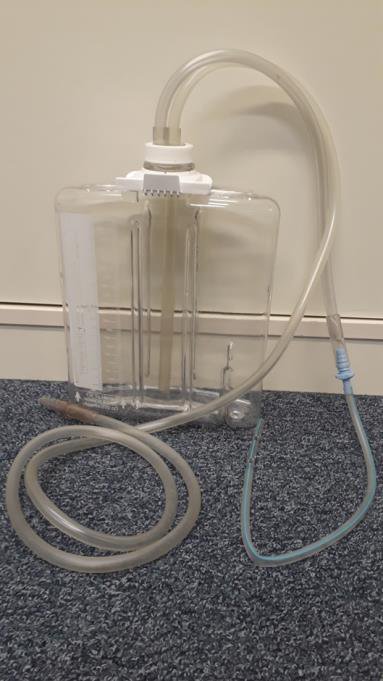
Your baby will also have a special tube called a ‘replogle tube’ passed through their nose or mouth into their oesophagus. This tube will allow the nurses caring for your baby to clear out the saliva that your baby cannot swallow. It is important that the Replogle tube is not pulled out, so your nurse might ask you to provide some mittens or socks that they can put over your baby’s hands to try and prevent this happening.
Your baby will not be able to have any milk, so they will be given fluids through one of their veins until an operation can be performed.
What happens before the operation?
The surgeon will explain the operation fully, and will talk through any concerns and questions you might have.
An anaesthetist will visit you to discuss the anaesthetic process that your baby will have during the operation. They will also talk through the pain relief that your baby will have during and after the operation.
The surgeon will ask for your written consent for the operation to go ahead. If you are unsure about anything, or have any questions to ask, please ask the surgeon before you sign the consent form.
What happens during the operation?
The operation is carried out under general anaesthetic. This means that your baby will be asleep throughout the operation.
You will be able to walk to the theatre with your baby. You might be able to go into the anaesthetic room with your baby, but sometimes babies, especially if they are very small or are on a ventilator to help their breathing, are taken straight into the operating theatre where it is warmer. In that case, you will not be able to escort them.
The operation is performed via a cut in the right side of the chest wall, or in selected cases might be performed laparoscopically (keyhole surgery). The surgeon will discuss the best operation plan for your baby. The distance between the two ends of the oesophagus will dictate which method is used to repair the oesophageal atresia. In most cases, the surgeon will firstly open the sealed end of the oesophagus at the top end that comes down from your baby’s mouth, and then join this to the end that connects to the stomach. This then forms a tube that allows for a continuous passage from throat to stomach.
To repair the tracheo-oesophageal fistula, the surgeon will separate the trachea from the oesophagus and then repair the part of the trachea where the oesophagus was originally joined. The two ends of the oesophagus are then joined as in the oesophageal atresia operation.
In rare cases, called ‘long gap oesophageal atresia,’ the gap between the two ends of the oesophagus is too large for the surgeon to be able to join them straight away. In this instance a different procedure and treatment is required. If this is likely to be the case for your baby, the surgeon will explain this to you.
What are the risks of the operation?
Surgical risks
Any surgery carries a small risk of bleeding or infection. Your surgeon will discuss these and any other risks with you before you sign to give your consent for the operation. All the doctors who perform this operation are specialists in this procedure.
Operations carry a small risk that the wound may not heal together as it should. In TOF / OA surgery, if the wound does not heal together, there is the risk of a leak along the repair of the defect (called an ‘anastomotic leak’). The medical and nursing staff will observe your baby closely for signs of this. Sometimes further surgery will be required.
Anaesthetic risks
In modern anaesthesia, serious problems are uncommon. While risk cannot be removed completely, modern equipment, training and drugs have made anaesthesia a much safer procedure.
The exact likelihood of complication is very much dependant on your baby’s medical condition and the nature of the surgery and anaesthesia they require. The anaesthetist can talk to you in detail about this prior to your baby’s surgery.
Are there any alternatives to an operation?
No, unfortunately OA and TOF will always require surgical treatment to enable your baby to feed.
What happens after the operation?
Your baby will be taken back to the neonatal unit after surgery, and will recover there. You will be able to see them as soon as they are settled back in their incubator. Your baby will initially require help with their breathing, and will be on a ventilator. They will also be given pain relief via a drip into their vein to allow them to rest and sleep.
After the operation your baby will be connected to monitors that measure their heart rate, oxygen levels and temperature. As your baby’s condition improves, the ventilation and monitors will be reduced, and they might be transferred into a cot.
Your baby will be regularly assessed for pain, and will be given pain medicine accordingly.
Your baby may have a tube inserted during surgery to drain any fluid or air that may be trapped. This is called a chest drain. This will be removed after a few days, when the surgeons and doctors are happy with your baby’s progress.


How will I feed my baby?
In order to allow the joins in your baby’s oesophagus and/or trachea to heal, it might be a while before your baby is allowed to take any milk orally. Initially your baby will be fed via one of the tubes in their vein (called parenteral nutrition, or PN). This will slowly be replaced by expressed breast milk or formula given through their nasogastric tube. As your baby recovers, and after an assessment by our speech & language team, milk will slowly be introduced orally, either from your breast or a bottle.
Please talk to your baby’s nurse regarding expressing your breast milk so that it is ready to use when your baby needs it; your nurse will explain how expressed milk is stored until it can be given to your baby.
Will I be allowed to be with my baby?
Although you will not be able to stay next to your baby overnight, the nurses on the ward will encourage you to participate in as much of your baby’s care as you feel able to. This can initially be very daunting when there are a lot of wires and drips attached to your baby, but it becomes easier with time. Please talk to your baby’s nurse if you are feeling overwhelmed.
When can we go home?
When your baby is feeding well, and is gaining weight, you will either be transferred to a hospital that is closer to your home, or discharged home. You will have regular visits from your health visitor or local community nursing team who will give you support and check that your baby is gaining weight. Details of your baby’s outpatient follow up appointment will be sent via post.
Are there any long term problems with this condition?
The majority of babies who have had OA and / or TOF without any other complications will go on to develop well. If your baby has been born with associated problems, their long-term development will depend on the severity of these conditions.
Breathing problems
Children born with OA / TOF very often have a very characteristic barking cough commonly referred to as ‘the TOF cough’. This loud, barking cough is caused by floppiness (tracheomalacia) of the trachea (windpipe). This cough sounds alarming, but is usually not serious. It can get worse during periods of illness, particularly when your child gets a cold or other respiratory problem. Children usually grow out of tracheomalacia by the age of two, and then only a minority of babies suffer severely.
Some babies with OA / TOF can experience periods when it appears that they are finding it hard to breathe. This is particularly likely to occur when a child is breathing heavily, for example when coughing or crying. Usually when the child calms down and relaxes, the airway opens up. Severe respiratory problems are rare, but if they occur, will require medical attention.
Children with OA / TOF may develop chest infections or asthma which, if serious, may mean your child needs to be admitted to hospital for a few days. The risk of this lessens as your child gets older. Avoiding smoking around or near your baby, and avoiding smoky places, can help.
Swallowing problems
Swallowing problems could occur due to the oesophagus narrowing (called ‘oesophageal stricture’) where it was repaired. If the narrowing is severe, your surgeon will recommend stretching it. This will be done in an operating theatre under general anaesthetic.
As they get older, children with OA / TOF often have abnormal swallowing patterns, and will have to learn, or might still be learning, to cope with their particular feeding problems. Some children will have problems swallowing certain foods. Your surgeon will recommend that they have a sip of drink between mouthfuls when they are eating to help with this.
Some children who have had OA / TOF will develop a problem with gastro-oesophageal reflux (GOR) when they are older. In GOR the contents of the stomach flow back up the oesophagus causing irritation and pain. If your child develops symptoms of GOR please speak to their surgeon or GP for further advice.
Discharge advice - How do I look after my child at home?
When should I contact the hospital?
You should call the surgical nurse specialist team at the hospital if your baby shows any of the following:
- Coughing or choking when feeding
- Difficulty in swallowing saliva or feeds including taking longer than usual to take a feed
- Is failing to gain weight.
Follow up
Your baby will be followed up as an outpatient in clinic throughout their childhood. You will be able to call the nurse specialist team with any concerns you might have about your child’s condition.
Chaperoning
During your child’s hospital visits your child will need to be examined to help diagnose and to plan care. Examination may take place before, during and after treatment, is performed by trained members of staff and will always be explained to you beforehand. A chaperone is a separate member of staff who is present during the examination. The role of the chaperone is to provide practical assistance with the examination and to provide support to the child, family member / carer and to the person examining.
Who should I contact if I have further queries, concerns or questions?
For further information / queries please contact:
Your nurse specialist (Monday to Friday 08:00 to 18:00): 01223 586973
The ward your child was on . . . . . . . . . . . . . . . . . . . . . .
Organisations that offer support and advice
Tracheo-Oesophageal Fistula Support (opens in a new tab) – supporting those born unable to swallow.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

