This leaflet is designed to provide dietary information for people living with liver disease, specifically for people diagnosed with liver cirrhosis.
The role of the liver
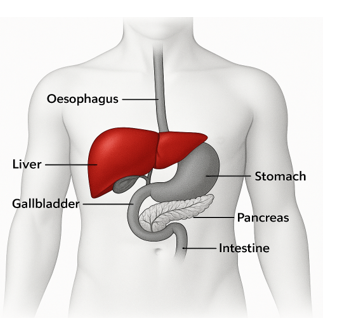
The liver is one of the most important organs in your body playing a critical role in your overall health. The liver is the only organ in the body which can heal itself. However, if there is prolonged damage this can lead to liver disease. The liver helps process the food you eat by turning nutrients into energy and storing vitamins and minerals. The liver also filters toxins and waste products from your blood, helping to keep your body clean and free from harmful substances. The liver also produces bile, a substance that helps with the breakdown of fats during digestion. The liver supports metabolism, helps regulate blood sugar levels, and plays a key role in maintaining your body’s overall balance and well-being.
Importance of good nutrition in liver disease
When you have liver disease your body requires extra energy (calories) and protein. Your body's requirements are higher as the liver has a major role in storing and releasing energy.
When you eat, the excess energy from your food your body does not need is stored in your liver as glycogen. Glycogen is an energy store the body makes, which it will use for times when we are not eating. This is to provide energy for your body’s vital functions. A healthy liver can store enough glycogen for up to 2-3 days of not eating. In liver cirrhosis the glycogen energy store is much smaller as the liver damage results in the liver not being able to make and store as much glycogen. This results in a glycogen energy store that lasts for only 2-3 hours after eating. After this time, the body has to look for a new source of energy and protein to fuel vital functions, so it starts to break down muscle to provide a new source of energy. This can lead to loss of strength, fatigue and weight loss, as well as worsening your overall symptoms.
Non-urgent advice: Recommendation
To prevent muscle wasting and worsening of these symptoms, we recommend you eat food including carbohydrates every 2-3 hours throughout the day and a 50g carbohydrate bedtime snack (see below). Also aim for good protein sources at each meal and snack.
Malnutrition is the lack or deficiency of essential nutrients and minerals needed by the body for health and to prevent muscle wasting and weight loss. In liver disease malnutrition has been reported in 20-50% of patients with a higher rate in people with decompensated liver disease. Decompensation is when your body is no longer coping with the scarring, and your liver is not able to function properly and you start to get symptoms of liver disease such as: jaundice (yellowing of the skin), ascites (fluid on the tummy), oedema (fluid on the legs), hepatic encephalopathy (confusion), and/or variceal bleeding
Malnutrition can present slowly over months or years but can also present quickly over a few weeks or months. Signs to look out for are rapid unexplained visual weight loss most notably in the arms, chest and face. For example, you may notice your arms of face getting slimmer. This suggests weight loss even if the scales do not change especially if you have any ascites or oedema. Muscle wasting can result in reduced exercise tolerance such as being unable to or struggling to climb the stairs, not being able to walk short distances or being unable to lift as much as you used to.
Causes of malnutrition in liver disease
- Decreased appetite
- Early satiety (feeling full quickly)
- Nausea and vomiting
- Malabsorption due to different things including loose stools
- Unnecessary diet restrictions
- All the above lead to not eating enough nutrients
Good nutrition helps to:
- Prevent muscle wasting and weight loss
- Maintain strength and mobility
- Prevent fatigue
- Promote wound healing
- Improve quality of life
- Prevent/reduce hospital admissions
- Fight and prevent against infections
- Manage ascites and encephalopathy
Carbohydrates
Carbohydrates are the body's main energy source. When you eat carbohydrates, they get broken down into glucose (sugar) which is then used to fuel the body. Some of this gets converted to glycogen and stored in the liver and muscles.
Starchy carbohydrates provide slow-release energy and should be included at each mealtime. If you have diabetes you may be worried about the effect this has on your blood sugar levels but it is still important to make sure you are getting enough carbohydrates throughout the day including before bed. Aiming to have more wholegrains may help to maintain your blood sugar levels throughout the day along with pairing carbohydrates with a source of protein and healthy fats. If you are concerned about or get high blood sugar levels please consult your dietitian and diabetes specialist nurse for advice on how to manage your blood sugar level.
Examples of Carbohydrates:
- Rice
- Bread
- Noodles
- Cereal
- Oats
- Pasta
- Potatoes and sweet potatoes
- Yam
- Couscous
- Chapatti
Carbohydrate bedtime snack
Having a carbohydrate-based bedtime snack provides the body with an energy source to use overnight to help prevent your muscles from being broken down due to the reduced glycogen store. Aim for this snack to contain 50g of carbohydrates. This ensures you have enough energy to fuel you overnight. Having a source of protein with this snack will help you achieve your protein goal. If you have diabetes and are worried about having a carbohydrate snack before bed please speak to your dietitian or diabetes specialist nurse for advice.
Carbohydrate bedtime snacks
- 2 sliced of bread/toast
- Bowl of cereal and milk
- Large glass of milk/milky drink and some biscuits
- Bagel, tea cake, crumpets and pancakes
- Cheese and crackers
- Cereal bar or popcorn (unsalted)
- Supplement drink prescribed by your dietitian
Healthier/Diabetic bedtime snacks
- Greek yoghurt, granola and fruit
- Boiled egg on toast
- Whole meal cereal with semi skimmed milk
- 2x slices of whole meal toast
- Supplement drink prescribed by your dietitian
Protein
Protein in the diet helps build and repair muscles. In liver disease your requirement for protein is higher. Having a high protein diet helps to prevent a loss of muscle mass and to help repair any muscle which has already been lost. Trying to have protein throughout the day in each meal and snack means the body is better able to utilize it.
Examples of protein
- Meat – try to aim for leaner cuts of meat
- Poultry
- Dairy products including dairy alternatives – note soya and pea milk often include more protein than other dairy alternatives
- Fish
- Eggs
- Pulses – peas, beans, lentils
- Meat alternatives e.g., Quorn, tofu, soya protein/mince, textured vegetable protein, fava beans, tempeh, seitan and edamame beans
Fruit and vegetables
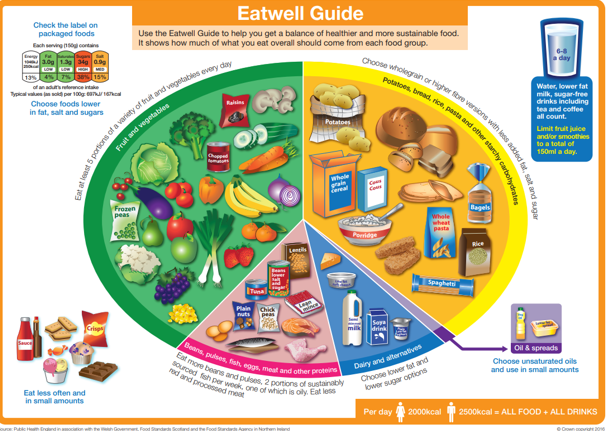
Fruit and vegetables help to provide the body with vitamins, minerals and fibre but tend to be lower in carbohydrates and protein. As part of a balanced diet try to aim for 5 portions of fruit and vegetables a day. If your appetite is suppressed or you have a low intake try not to fill yourself up on these.
Below is a copy of the Eatwell Guide with advice on how to achieve a balanced diet by eating the right proportions of different food groups including lots of fruits, vegetables, wholegrains, protein, and limit foods high in fat, salt, and sugar.
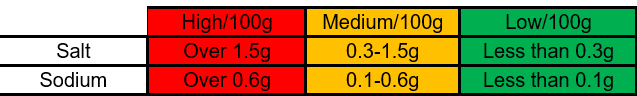
Salt
In liver disease fluid can collect around your abdomen (ascites) as well as body tissues often feet, ankles and legs (oedema). Limiting the amount of salt in your diet can help to reduce fluid retention and decrease ascites and oedema.
Aim for less than 5g of salt a day
Tips to help reduce salt in your diet:
- Avoid adding salt when cooking meals
- Avoid adding extra salt to meals once cooked
- Check food labels – aim for green or amber
- Add extra seasonings – herbs, spices, pepper, garlic and sauces
The table below shows you how to read food labels to see the salt content of food:
| Food type | Flavouring Suggestions (No Salt) |
|---|---|
| Food type Vegetables | Flavouring Suggestions (No Salt) Garlic, onion, lemon juice, balsamic vinegar, black pepper, dill, rosemary, thyme, basil, mint, paprika |
| Food type Poultry | Flavouring Suggestions (No Salt) Garlic, onion, lemon zest, tarragon, sage, thyme, rosemary, smoked paprika, black pepper |
| Food type Beef | Flavouring Suggestions (No Salt) Black pepper, garlic, onion powder, rosemary, cumin, coriander, smoked paprika, mustard |
| Food type Pork | Flavouring Suggestions (No Salt) Fennel, sage, thyme, garlic, clove, cinnamon, mustard |
| Food type Fish & Seafood | Flavouring Suggestions (No Salt) Lemon juice, dill, parsley, tarragon, fennel, black pepper, garlic, lime zest |
| Food type Eggs | Flavouring Suggestions (No Salt) Chives, black pepper, chilli, garlic, dill, paprika, |
| Food type Soups & Stews | Flavouring Suggestions (No Salt) Bay leaves, thyme, oregano, smoked paprika, garlic, onion, celery |
| Food type Grains (rice, etc.) | Flavouring Suggestions (No Salt) Turmeric, cumin, coriander, garlic, ginger, lemon zest, onions, parsley |
| Food type Pasta | Flavouring Suggestions (No Salt) Basil, oregano, garlic, chillies, lemon juice, black pepper |
| Food type Pulses (beans, lentils) | Flavouring Suggestions (No Salt) Cumin, coriander, chili, garlic, smoked paprika, onion, bay leaf |
| Food type Tofu & meat alternatives | Flavouring Suggestions (No Salt) Ginger, garlic, chili flakes, lime juice |
| Food type Salads | Flavouring Suggestions (No Salt) Lemon juice, balsamic vinegar, mustard, herbs, garlic, avocado |
Supplement drinks
Due to increased requirements and often a lower oral intake, it is harder to meet energy and protein requirements through diet alone. In this case your Dietitian may suggest supplement drinks to help prevent weight and/or muscle loss and help to build you up. There are lots of different brands and types of supplement drinks on the market so your dietitian will work with you to find the best one dependent on your needs. Please note that if you are admitted to hospital your prescription at home may be different.
If you are struggling to have snacks or a meal every 2-3hours, you can drink your supplement drinks at this point as your body will use them the same as food. This will stop you going for long periods of time without food and help to preserve your muscles.
If you are someone with diabetes please speak to your dietitian for advice on how to ensure these do not cause spikes in your blood sugar levels.
Tips for taking supplement drinks
- Storing them in the fridge
- Serving them over ice
- For milk style drinks you can add milk to thin them out
- For juice style or protein supplements you can add water, sparkling water, lemonade or juice to thin them out
- Try freezing them to have as an ice cream/ice lolly
Non-urgent advice: Suggested meal plan
- Breakfast
-
- Cereal with milk
- Porridge/overnight oats
- Greek yoghurt with fruit
- Toast with eggs/beans/peanut butter
- Mid- morning
-
- Yoghurt
- Hummus with cracker/pitta/veg sticks
- Cheese and crackers
- Toast/crumpet/scone
- Biscuits or cereal bar
- Glass of milk
- Supplement drinks – if you are prescribed these
- Lunch
-
- Ensure your meal is balanced and includes a source of protein (e.g., cheese, chicken, fish, meat, pulses, meat alternatives), a source of carbohydrate (e.g., pasta, bread, rice, chapatti, potato) and vegetables of your choice
- Meal examples include: jacket with tuna or beans, soup and a roll, spaghetti bolognaise, salad (ensuring has protein and carbohydrates), chicken chickpea curry
- Optional dessert (check with your dietitian first) - yoghurt, rice pudding, cake, fruit and cream, ice cream, crumble
- Mid-afternoon
-
- Yoghurt
- Hummus with cracker/pitta/veg sticks
- Cheese and crackers
- Toast/crumpet/scone
- Biscuits or cereal bar
- Glass of milk
- Supplement drinks – if you are prescribed these
- Dinner
-
- Yoghurt
- Hummus with cracker/pitta/veg sticks
- Cheese and crackers
- Toast/crumpet/scone
- Biscuits or cereal bar
- Glass of milk
- Supplement drinks – if you are prescribed these
- Bedtime snacks
-
See section earlier in the leaflet
* Please note the above table is just an example of foods you could have.
Exercise
Regular physical activity is important for everyone’s health, especially for those with liver disease. The NHS recommends at least 150 minutes of moderate aerobic activity per week plus two days of muscle-strengthening exercises. Try starting gently (even 10 minutes counts) and building up, as well as discussing activity options with your doctor, especially if you feel fatigued or have symptoms. Please make you do this to your own physical and medical ability.
Please note if you have been advised to lose weight or are on weight loss medication, please speak to your dietitian for advice to ensure you do not lose muscle mass.
The British Liver Trust provides information and support for everyone affected by liver disease visit the British Liver Trust website (opens in a new tab) or call 0800 652 7330.
Contact details
Main office telephone: 01223 216655
My Chart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device
More information is available on the My Chart section of our website.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

