Introduction
Your child has been diagnosed as having gastro oesophageal reflux disease (GORD) for which medication has given little or no relief. This means that stomach contents are refluxing (going back up) the oesophagus (food pipe). If GORD is left untreated the regular refluxing of the stomach’s contents can cause damage to the lining of the oesophagus. In addition, reflux can cause other problems such as chest infections due to aspiration (aspiration pneumonia), pain and/or vomiting and your child may fail to gain weight.
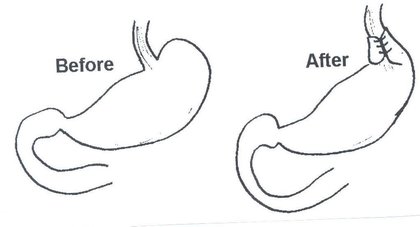
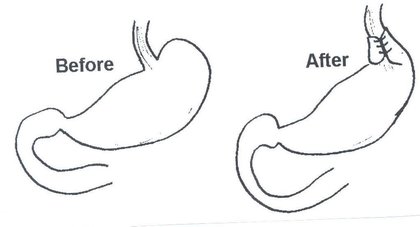
What is a fundoplication?
A fundoplication, also known as anti-reflux surgery, is a surgical procedure used to treat GORD where the medical therapy has failed. The operation involves using the top part of the stomach called the fundus. The fundus is wrapped around the bottom part of the oesophagus to tighten the junction between the oesophagus and the stomach. After a fundoplication, when your child eats/drinks and the pressure in the stomach rises as it fills up, the junction closes off and the contents will no longer be pushed back up the oesophagus.


Preparation before admission to surgery
Before surgery takes place the following will occur:
1 - Contrast study
Your child will need to have undergone an x-ray called a contrast study. This involves your child taking some contrast (dye) by mouth or, if your child has a feeding tube, the contrast can be given via the tube. The contrast outlines the stomach and also the first part of the bowel when the x-ray is taken.
This allows the surgeon to see an image of your child’s anatomy before operating. This is important because occasionally the bowel or stomach can be in a different position than is usual and it is important to know about this before the operation begins.
2 - Pre-operative assessment
You will be asked to complete a health screening questionnaire when your child is added to the waiting list; this will be completed immediately after your appointment if your child was seen in one of our clinics at Addenbrooke’s or, over the telephone if your child was reviewed in one of our outlying clinics.
3 - Blood tests
Blood tests will be required and these are taken within four weeks of the operation date.
4 - Dietician
Your child will be referred to one of our paediatric dieticians who will then visit you and your child on the ward after surgery has taken place.
Admission to hospital
You will be asked to bring your child to one of our children’s wards. For most children this will be early in the morning on the same day as the operation but occasionally, this may be one day prior to surgery if your child has an underlying condition which means they need monitoring before surgery. You will be met by nursing staff and seen by your doctors and anaesthetist. Whilst you child is in hospital you will be able to stay with your child overnight if you wish. You can also be present while your child goes to sleep for their operation, and in the recovery area where he/she wakes up.
The operation
The operation will be carried out under a general anaesthetic. Most children will have their fundoplication carried out as a laparoscopic or minimally invasive procedure (key-hole surgery). Small, usually five, key holes (about 5mm long each) are made in the tummy wall. Through these holes, special instruments are used to perform the surgery and wrap the fundus of the stomach around the bottom of the oesophagus. This is all visualised on a TV screen by a miniature camera which is inserted through one of the key holes. After a laparoscopic Nissen’s Fundoplication some children may require monitoring on our paediatric high dependency or intensive care unit but others will be able to return to our children’s ward. Children need to remain in hospital for approximately two to four days whilst they start feeding again.
How is this operation different from a traditional one?
The actual procedure is the same. The only thing that is different is the way in which we get to the stomach. In traditionally surgery, a cut approximately 10 to 15cms long was/is made. This takes longer to heal than the little holes of key hole surgery, increases postoperative pain and length of hospitalization and makes and the recovery is slower.
Is there a guarantee that key hole (laparoscopic) surgery can be done?
No, it is not possible to guarantee that the operation can be completed by key-hole surgery. If there is some technical difficulty which may lead to an unsafe procedure (for example, it is difficult to visualise the stomach or the wrap) then a traditional cut will need to be made. The stay in hospital will be longer (approximately five to seven days) as well as the recovery at home.
The chances of having to convert to open surgery are small, about 5%. If your surgeon does not feel that key hole surgery is suitable in your child’s case, (for example due to previous abdominal surgeries or other comorbidities), this will be discussed this with you at your outpatients appointment.
What are the risks / complications of surgery?
As with all operations there are risks but these are rare. They include:
- Bleeding, bruising, infection and/or protrusion of tissue through the wound affecting one or more of the key hole incision sites.
- Failure/recurrence and retching - There is an approximate 5% failure rate associated with this operation. Failure is usually due to the wrap coming undone or being stretched enough to allow reflux to reoccur. Constant retching is a risk factor in the wrap becoming stretched. Unfortunately retching cannot always be controlled by medication. If the wrap does become stretched or undone, further surgery may be needed.
- Gas bloat - (See section on care after a fundoplication).
- Adhesions - This is scar tissue formation which can occur after any abdominal operation. It is a small but lifelong risk which may result in an obstruction (blockage) of the intestine. Symptoms of an adhesion obstruction include cramping abdominal pain and green (bile) vomit.
- Dysphagia -Occasionally children can experience swallowing difficulties (called dysphagia) after having a Nissen’s Fundoplication and get the sensation that food is stuck. To help with this it is important that the diet is altered as described below. Usually any swallowing difficulties resolve over time as the swelling resolves but rarely further intervention may be needed, for example, an endoscopy (passing a camera down the food pip) and gently stretching the wrap slightly.
- Dumping - Dumping is a rare complication after fundoplication surgery. Gastric dumping is a term used to describe rapid stomach emptying. Food leaves the stomach too rapidly and enters the intestine largely undigested. Symptoms include nausea, bloating, cramping pain, dizziness and diarrhoea and sometimes low blood sugar levels can occur. If you are concerned that your child may have symptoms of dumping it is important to call the surgical care team or dietician as further alterations to diet may be needed.
- Retching - Some children, like adults, can feel sick after having an operation or general anaesthetic. Retching can stretch the Nissen’s wrap so that it becomes ineffective so, if your child is feeling nauseous immediately after surgery a nurse can give medicines to help ease this and so prevent retching. Occasionally children will continue to retch in the longer term. This may because of an underlying condition or because your child is unable to tolerate their feeding regime. It is important that you contact the surgical team if retching is ongoing. Changes to a feeding plan may be needed or further treatments or interventions arranged.
What happens immediately after the operation?
- You will be able to be with your child as soon as they begin to wake in the recovery room; we provide you with a device called a pager which will inform you when your child is in the recovery area and awake. Once your child has fully woken, she/he will be taken back to the ward. Some children (for example children with known chest or neurological problems) will need to be monitored in the high dependency unit before then being transferred back to the ward.
- Local anaesthetic will be used at the end of the operation to stop pain from the key holes. However, some children experience some discomfort around their tummy muscles and shoulders from the gas that is used in laparoscopic surgery. This will be relieved by your child being given pain killers through a drip or as suppositories (once your child starts drinking, medicine can be given by mouth).
- Some children need to be monitored in our children’s high dependency or intensive care unit after surgery but others are transferred back to our children’s ward.
- Until your child is able to feed again, fluid will be provided by a drip which will have been inserted during the operation.
- Your doctors will tell you when your child will be able to start drinking/eating again. Many children are able to start having sips of water a few hours after their operation but some children will not start having water for a few days. Once fluids are being tolerated he/she will be allowed to start eating (see the section on diet below).
Care after a fundoplication
1 - Recommencing feeding
Your doctors will tell you when your child will be able to start drinking and eating again. Most children who fed by mouth before surgery will be able to start having sips of water a few hours after their operation then start drinking more and eating again the following day. For children that were fed by a feeding tube before surgery, feeds will re-start via the feeding tube on the day after surgery.
2 - Alteration in diet
- Because the fundus of the stomach has been used to make the wrap, the overall size/capacity of the stomach is temporarily reduced (by about 10%). It is therefore necessary that there is some alteration in your child’s diet after surgery and that their diet is gradually returned to their normal over a period of weeks.
How this is managed depends on whether your child ate my mouth or was fed by a feeding tube before surgery:
For children who ate by mouth before surgery:
- As the fundus of the stomach has been used to tighten the junction between the oesophagus and the stomach, swallowing lumps will be difficult in the first weeks after surgery. All children will need to have a pureed diet for the first few weeks (minimum of two).
- A pureed diet means eating foods in a liquidised form so you will need a food blender or liquidiser. The ideal consistency of pureed food is smooth and moist, like plain yogurt.
- The table below lists foods that are readily suitable as pureed food and others that need to be liquidised first:
| Food group | Readily suitable foods | Foods that need liquidising first | Unsuitable foods |
|---|---|---|---|
| Breads and cereals | Readily suitable foods Smooth porridge such as Ready Brek, Weetabix (mixed to a paste) | Foods that need liquidising first Other breakfast cereals | Unsuitable foods Toast |
| Potatoes | Readily suitable foods Mashed potato with lots of butter / cream | Foods that need liquidising first Boiled potatoes | Unsuitable foods Roast potatoes, chips |
| Biscuits, cakes, snacks | Readily suitable foods | Foods that need liquidising first Soft cake, pureed down with custard / cream | Unsuitable foods Biscuits, other crisps, nuts |
| Meat / Fish / Alternatives | Readily suitable foods | Foods that need liquidising first Steamed / mashed / poached meat or fish, minced meat | Unsuitable foods Dry meats such as roast chicken, turkey or beef |
| Dairy foods | Readily suitable foods Cottage cheese, cheese spread, yoghurt with no lumps, all types of milk | Foods that need liquidising first Grated cheese, yoghurt containing fruit pieces | Unsuitable foods Hard cheese |
| Fruit and vegetables | Readily suitable foods Pureed sieved vegetables, stewed fruits, hummus, mushy peas | Foods that need liquidising first Mashed / diced fruit and vegetables | Unsuitable foods Vegetables with tougher skins such as Sweetcorn, baked beans, peas |
| Eggs | Readily suitable foods Egg mayonnaise | Foods that need liquidising first Boiled / fried / scrambled / poached egg | Unsuitable foods |
| Desserts | Readily suitable foods Mousses, semolina, rice pudding, ice cream, custard, jelly, fruit fool | Foods that need liquidising first Soft cakes pureed with cream or ice-cream | Unsuitable foods Pastry based desserts |
After approximately two weeks your child can start to have mashed foods and then, gradually, over a period of some weeks, the consistency of food can be gradually built up. (The exact time frame will be different for each individual child but your dietician and surgical team will oversee a plan for your child). Dry foods such as chicken will be introduced last and will need to be eaten with lots of gravy/sauce to prevent it getting stuck in the food pipe.
If a lump of food is eaten which cannot pass down into the stomach your child will usually retch it back up. If this does not happen you should seek medical advice without delay.
If food getting stuck becomes a severe/prolonged problem further surgery may be required.
For children who were fed via a feeding tube before surgery
- To start with your child will receive their feed as a continuous feed via a feeding pump rather than as boluses.
- The rate (speed) of the feed will be gradually increased and, at the same time, the rate of the intravenous fluid drip reduced.
- Once full continuous feeding has been established the intravenous fluid drip will be discontinued and your child can begin to take their feeds as a mixture of continuous and slow bolus feeds.
- It is likely that your child will be ready for discharge before they have returned to their usual feeding regime so your dietician will provide you with a plan to follow at home which gradually changes towards a longer term regime.
3 - Gas bloat
- After a fundoplication it can be difficult for your child to burp. If your child is unable to burp up gas the stomach becomes distended. In most children this does not cause a significant problem and the gas passes through the gut. However, gas bloat can make some children feel unwell with symptoms of trapped wind (for example, pain, feeling bloated) and occasionally children can feel very poorly and become pale and sweaty.
- If gas bloat occurs and they have a feeding tube in place, the air can be removed through this. Your child’s nurse will teach you how to remove trapped air through the tube to relieve gas bloat.
- In children who feed orally, to help prevent gas bloat food should be eaten slowly and chewed well prior to swallowing.
- If gas bloat becomes a problem after discharge from hospital you should contact your nurse specialist/dietician for advice.
4 - Medications
- Your child may have some discomfort and should be given pain killers such as children’s paracetamol and/or Ibuprofen regularly. It is important that you follow the instructions on the bottle.
- Although your child will not be experiencing reflux any more, their oesophagus (food pipe) needs to heal and so children should continue to take any anti-reflux medication that they were taking before surgery until they return for out-patient review. It is usual for the anti-reflux medication to then be discontinued, usually one at a time.
5 - General discharge advice
- As the stitches are dissolvable they do not need to be removed.
- Your child can have showers but baths are not permitted for five days.
- Where dressings have been applied, these can be gently pulled off after seven days (it is easiest and less painful to do this in the bath).
- Your child should rest at home for two weeks.
- Wound infections are rare but if your child’s wound looks red/sore see your GP.
- If your child develops a fever or pain that is not helped by pain killers provided, you should contact your nurse specialist/GP.
Chaperoning
During your child’s hospital visits your child will need to be examined to help diagnose and to plan care. Examination may take place before, during and after treatment, is performed by trained members of staff and will always be explained to you beforehand. A chaperone is a separate member of staff who is present during the examination. The role of the chaperone is to provide practical assistance with the examination and to provide support to the child, family member/carer and to the person examining.
Follow up
You will receive an appointment to attend the outpatients department approximately six to 12 weeks after your child’s operation for review.
For further information/if you have any queries, please contact:
The ward you were on:
Your nurse specialist: 01223 586973
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

