Introduction
Patients who have had a diagnosis of Heart Failure confirmed by a Cardiologist and have been referred to the Heart Failure Specialist Nurse team will be given this booklet.
The aim of this booklet is to provide information regarding your diagnosis, and also to advise you how to recognise and manage symptoms related to Heart Failure.
Who we are
We are the Addenbrookes Integrated Nurse-Led Heart Failure Team.
We are a team of Specialist Cardiology Nurses, who help people diagnosed with Heart Failure to manage their symptoms and to stay well.
We are an Integrated Team, which means we help patients admitted with symptoms of Heart Failure, as well as supporting people living with this condition at home.
We work closely with our Cardiology Consultant colleagues, who provide advice or support when required.
We have an Administration Team to support our work, who help book your appointments.
Please be aware that we are only able to support patients who are referred to our service. The referral to our service is via GP, General Cardiology and other specialist services.
What the service provides
The Heart Failure Service provides support in several ways. This support is available face-to-face, via telephone and also online.
After each consultation with the Heart Failure Specialist Nurse, we will ensure your GP is kept informed of any changes we have made to your management.
We are a specialist service, which means that we provide support while it is required. Once your symptoms are stable, our routine input will end, however your GP can refer you back to our service if our support is required again.
We offer support in the following ways:
Education - to help you understand your condition.
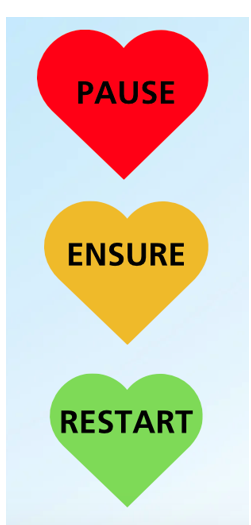
Support and advice - to help you when symptoms have increased.
Medication reviews - to ensure you are on the correct medication, and to provide the best outcomes for you.
Referral to other specialist teams. - These include Cardiac Rehabilitation, Breathlessness Intervention Service or Palliative Care (If required).
Links to Consultant Cardiologist Colleagues - We have regular meetings with our consultant colleagues.
Why you are attending this clinic
If you are attending our Clinic, you have been referred either by your GP or these other services.
Whilst you are in hospital - You were admitted to hospital due to symptoms of Heart Failure. While in hospital your diagnosis was confirmed by a Cardiologist. Or you may already be known to a Cardiologist.
Following GP Review - Your GP referred you to our service due to a suspected diagnosis of Heart Failure, or worsening symptoms of known Heart Failure. This referral was accepted, and you were seen in Clinic by a Cardiologist who confirmed your diagnosis and referred you to our Clinic.
Following Cardiology Review or Other Specialist Services - Your diagnosis of Heart Failure was confirmed, and this was explained to you in Consultant Clinic.
Heart failure specialist nurse-led clinics
There are a range of clinics available. (Education / Ambulatory Care/ Medication Optimisation). We will refer you to the correct clinic. You may be switched between clinics if this is required.
Education - Guides you through the initial stages of diagnosis, supporting you to manage your condition independently. These clinics are available as Face to Face or telephone consultations, or online.
Ambulatory Care - Allows closer monitoring and can help prevent prevents potential admission to hospital if symptoms become problematic. Attendance can be up to 3 times per week. We are able to adjust oral medications and can administer intravenous diuretics (medicine to reduce fluid levels in the body) and can refer you for Intravenous Iron infusions if these are required.
Medication Optimisation Clinic - For patients with reduced Left Ventricular function (HFrEF) only. These clinics allow adjustments to your medications to ensure you are on the best available combination. You will be seen in Clinic, at 1-2 weekly intervals, until your medication is optimised.
Brief Intervention Calls - Our Helpline is available to all patients on our caseload. These calls respond to voicemail messages left for our service. The voicemail is checked 3 times per day, Monday-Friday.
| Date | Weight | Date | Weight | Date | Weight |
|---|---|---|---|---|---|
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
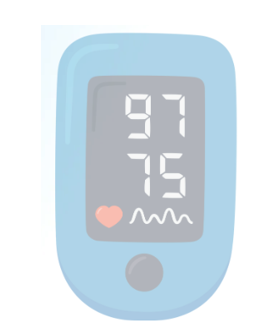
| Date | B/P | Pule | Date | B/P | Pule |
|---|---|---|---|---|---|
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
Heart failure or cardiology resources
Pumping Marvellous (opens in a new tab) (opens in a new tab) or 01772 796542
British Heart Foundation (opens in a new tab) (opens in a new tab)
British Society for Heart Failure (opens in a new tab) (opens in a new tab)
The Breathlessness Intervention Service or 01223 349325
Heart Failure Matters (opens in a new tab) (opens in a new tab)
Medication Resources
Dapagliflozin (opens in a new tab) (opens in a new tab)
Sacubitril/Valsartan (Entresto) (opens in a new tab) (opens in a new tab)
Other Heart Failure Medications (opens in a new tab) (opens in a new tab)
Older Adults Resources
Age UK (opens in a new tab) (opens in a new tab)
Cambridgeshire County Council (opens in a new tab) (opens in a new tab)
Non-Cardiology Resources
Psychological Wellbeing Service (IAPT) (opens in a new tab) (opens in a new tab) or 0300 300 0055
Hospice UK (opens in a new tab) (opens in a new tab) /Information and Support (opens in a new tab) (opens in a new tab)
Sue Ryder palliative, neurological and bereavement support (opens in a new tab) (opens in a new tab)
Arthur Rank Hospice (opens in a new tab) (opens in a new tab) or 01223 675777
MyChart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device
More information is available on our website: MyChart
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/