What are deep vein thrombosis and pulmonary embolism?
It is essential that blood remains fluid within the circulation but clots at the site of an injury. Blood should not clot within a healthy normal blood vessel. Thrombosis is the name given to a blood clot within a blood vessel.
Deep vein thrombosis (DVT) is the name given to blood clots forming within the deep veins. The most common site for a DVT is the deep veins in the legs.
A clot below the level of the knee is called a calf-vein DVT or distal DVT. A clot behind the knee or above the knee is called a proximal DVT.
A DVT can occasionally affect other veins in the body.
When a DVT forms, pieces of the clot can break away and pass through the circulation and lodge in the blood vessels in the lungs. These vessels are known as pulmonary arteries. This type of clot is termed a pulmonary embolism (PE).
When a PE occurs, the piece of clot that has broken away from the DVT often breaks into small pieces when it enters the pulmonary arteries (blood vessels in the lungs) and this causes multiple defects on the lung scan. Therefore, it is usual for the diagnostic scan (usually a CT scan or VQ scan) to show ‘multiple PEs’. The number of PEs on the scan at diagnosis does not usually affect treatment.
Deep vein thrombosis (DVT) and pulmonary embolus (PE) are collectively known as venous thrombosis (VT) or venous thromboembolism (VTE).
Why do DVT and PE occur, and what is the difference between a provoked and an unprovoked clot?
The blood clotting process is a delicate balance; blood should remain fluid within the circulation but clot at the site of an injured blood vessel. The balance can be shifted towards clotting, so clotting actually occurs in the circulation within a blood vessel, this is thrombosis. In about half of the patients who develop a DVT or a PE the clotting balance has been shifted by something which we call a provoking factor. When a provoking factor is identified we call this a provoked DVT.
Recognised provoking factors include, but are not limited to:
- Hospitalisation in the previous three months, including operations.
- Major trauma including major fractures.
- Pregnancy.
- Oral contraceptive use and hormone replacement therapy.
- Occasionally, immobilisation for at least several days
- Cancer
Patients who suffer a calf-vein DVT are at low risk of a clot occurring spontaneously in the future, regardless of whether it was provoked or unprovoked and so they are treated with anticoagulant therapy for only twelve weeks. Patients who suffer a very clearly provoked proximal DVT or a PE are at relatively low risk of a clot occurring spontaneously in the future and so they are treated with anticoagulant therapy for 12 weeks. Patients who suffer an unprovoked proximal DVT or a PE may be at risk of a clot occurring spontaneously in the future and we think about long-term anticoagulation to prevent further clots. These patients are seen in the Thrombophilia clinic whilst on anticoagulant treatment. The purpose of this clinic appointment is to begin to investigate their risk of further clots and produce a personalised care plan. In some patients where there is a weak provoking cause for the clot then we also might think about long-term anticoagulation in the Thrombophilia Clinic, as there can be a risk of a clot again in the future. All patients who have had a previous DVT/PE will be seen in the thrombophilia clinic whilst on anticoagulation therapy.
How is my DVT or PE treated?
Once a diagnosis of DVT or PE is made, anticoagulant therapy is started by either;
Giving an oral anticoagulant such as rivaroxaban, edoxaban or apixaban which acts immediately. These are given at a fixed dose. We do not need to monitor levels of these medications.
Or
Giving warfarin, an alternative oral anticoagulant tablet offered when others are unsuitable. Warfarin takes up to five days to work at the desired anticoagulant (blood thinning) effect when started or after dose changes. The injectable anticoagulant drug heparin is given at the same time while warfarin starts to work. When warfarin is working the heparin is stopped. Patients on warfarin need to have a regular blood test known as an International Normalised Ratio (INR) test. We will provide you with additional information if you are prescribed warfarin.
If you have been given a stop date for your anticoagulation therapy you should stop on the date instructed. You do not need to reduce the dose gradually, you just stop it. When you stop warfarin you do not need any more INR tests. You do not need to be seen in the Thrombophilia clinic and an appointment will not be made.
Should I take any special precautions in the future?
After a DVT or a PE you can reduce any risk of a further clot by:
- Improving your general level of fitness and mobility.
- Reducing your weight if your BMI is above 30kg/m2.
- Stopping smoking if you are a smoker.
- Avoiding the use of oestrogen-containing hormones including combined oral contraceptive pills (COCs) and hormone replacement therapy (HRT).
Women who become pregnant should inform their GP or midwife as they would usually need to start daily injections of low molecular weight heparin and be referred for hospital care in a pregnancy.
If you are hospitalised you must inform the doctors and nurses that you have previously had a DVT or a PE. They can arrange simple treatment (usually with a course of anticoagulation) to reduce your risk of a further clot. This includes after an operation or if you have your leg immobilised after injuring it or breaking it (as this can be risky for a DVT).
Travelling and thrombosis risk
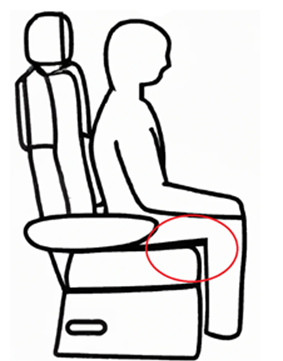
There is evidence that long distance travel is a risk factor for the development of thrombosis (blood clots). It is often described as traveller's thrombosis, thought to be caused by prolonged immobility and seat-edge pressure on the back of the legs illustrated in the figure below.
It can occur in association with any form of long-distance travel, by car, bus, rail, ferry or plane. The longer the length of travel the greater the risk of blood clots forming in a deep vein. There are precautions you may consider to minimise your risk of both deep vein thrombosis (DVT) and pulmonary embolism (PE) for continuous journeys lasting more than 4-6 hours.
Measures to reduce the risk of thrombosis for all travellers
Maintain your mobility; do not sit for long periods, particularly with pressure on the back of your thighs. Avoid crossing your legs when sitting and make frequent changes of position, such as taking a walk.
Avoid sleeping tablets as they may also contribute to longer periods of immobilisation. Regularly flex your ankles to contract your calf muscles.
Maintain hydration by drinking plenty of water and soft drinks and minimising alcohol and caffeine intakes. Remember that air conditioning, excess heat, diarrhoea and vomiting and inadequate fluid intake can all cause dehydration.
Moderate risk group
You have a moderate risk of developing thrombosis if you have any of the following:
- Have had a DVT /PE in the past
- Have had trauma or surgery with a general anaesthetic lasting more than 30 minutes in the previous two months, but not within the last four weeks
- Are obese (defined as a body mass index above 30kg/m2)
- Have varicose veins
- Are pregnant or in the 6-week post-partum period (after birth)
- Are taking oestrogens, such as oral contraceptives or hormone replacement therapy (HRT)
- Aged over 60 years
- Extremes of height. Taller than 1.9m (6ft 2in) or shorter than1.6m (5ft 3in)
- Have inherited blood clotting abnormalities
- Limited mobility (for example a lower limb fracture)
- Medical illnesses such as active inflammatory bowel disease, severe heart failure or infection
- Polycythaemia
Measures to reduce the risk of thrombosis for travellers in the moderate risk group
Follow the recommendations above for all travellers. Wear well fitted below knee compression hosiery, which are also called travel socks and provide 15-30 mmHg of pressure at the ankle (check this with your healthcare professional or the product merchant).
High risk group
You have a high risk of developing thrombosis if you have any of the following:
- Have had a surgical procedure under general anaesthetic lasting more than 30 minutes in the last month
- Have active cancer
Measures to reduce the risk of thrombosis in the high risk group
Follow the recommendations above for all travellers.
Wear well fitted below knee compression hosiery, which are also called travel socks and provide 15-30 mm Hg of pressure at the ankle. (Check this with your healthcare professional or the product merchant).
Ask your GP to consider prescribing appropriate anticoagulant medication to help reduce your risk of thrombosis either:
- Low molecular weight heparin (LMWH) subcutaneous injection (such as dalteparin) may be given by self-administration one to two hours prior to the start of the journey.
Or
- Rivaroxaban 10mg tablets orally with food one to two hours prior to the start of the journey. Tablets may be crushed and mixed with 50mL water for patients with swallowing difficulties.
Any person who has recently had a DVT/PE diagnosed and is taking anticoagulant therapy should seek advice from their doctor if taking long distance travel within four weeks of diagnosis.
The risk of developing travel related DVT or PE is small. You can benefit from following suggestions on how to minimise your risk.
Anyone who develops pain or swelling in their legs, chest pain and/or shortness of breath after a long journey should seek medical advice.
Aspirin has not been shown to be effective in reducing the risk of traveller's thrombosis.
Any person on oral anticoagulation is already taking pharmacological precaution against the development of thrombosis and should still follow other precautionary measures listed above such as maintaining hydration and mobility.
What are the symptoms of a DVT or PE that I should look out for in the future?
Symptoms of a DVT may include: pain, tenderness, swelling, warmth, redness, unexplained ache in leg. You can have a DVT without leg swelling.
Symptoms of a PE may include: feeling out of breath, coughing up blood, sharp stabbing pain in the chest or collapsing.
If you are concerned you may have a blood clot, it is very important that you seek urgent medical attention.
Information for women
Advice regarding periods
If you are on blood thinners you may have heavy periods, unfortunately this is quite common. Please book a GP appointment to review this if needed and the GP can seek specialist hospital advice if required.
Advice regarding hormone therapy
Tablet hormone replacement therapy (containing oral oestrogen), some injectable progesterone’s, the combined oral contraceptive pill (containing oestrogen) and norethisterone tablets increase the risk of blood clots and generally should be avoided if you are not taking anticoagulant medication.
The mini-pill, coil (including Mirena) and patch / gel / spray hormone replacement therapy do not increase clot risk and can be taken if you have previously had a clot.
What about pregnancy?
Pregnancy increases the risk of blood clots and this can last until 6 weeks after the delivery.
In women that have previously had a blood clot and become pregnant, injections of preventative (prophylactic) low-molecular weight heparin (LMWH, an injectable blood thinner which is safe during pregnancy and breast feeding), should start as soon as you find out you are pregnant and this usually continues until 6 weeks after the delivery. Your GP or midwife should also refer you to the local obstetric services for review.
You should look out for symptoms of blood clots in pregnancy too. (See previous section). We advise not becoming pregnant for at least 3 months after a blood clot diagnosis.
If you are planning a pregnancy please ask for a referral to the obstetric haematology clinic if you would like to discuss pregnancy and clot risk.
Lots more information is available on Thrombosis UK website. visit: thrombosisuk.org
Patient preferences and allergies
Heparin comes from animals. If you have any concerns about using animal products, please tell your doctor and they will discuss other options with you.
Please inform your doctor if you have an allergy to latex as dalteparin products also contain latex and alternative latex-free options are also available.
Keep all medicines out of sight and reach of children.
My Chart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device
More information is available on the MyChart section on our website.
Contacts
Cambridge University Hospitals anticoagulant service
Telephone: 01223 217127
References
NICE guideline 158, venous thromboembolic diseases: diagnosis, management and thrombophilia testing. March 2020, updated 2023
NICE guideline 89, venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. March 2018, updated 2019
NICE clinical knowledge summary, DVT prevention for travellers. Revised 2023
NICE guideline 23, menopause: identification and management November 2015, updated 2024
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

