Community Diagnostic Centres (CDCs) have been introduced to reduce the current waiting lists following the Covid-19 pandemic and to make diagnostic imaging more accessible to everyone by situating these facilities in the community. This service is overseen by Cambridge University Hospitals (CUH) NHS Foundation Trusts.
What is a lung function test?
Our lung function unit undertakes several physiological assessments to aid with the diagnosis of lung conditions like asthma, Chronic Obstructive Pulmonary Disease (COPD).
Prior to your appointment please do not use any inhalers for 24 hours.
The reason we ask you to stop your inhalers is so we can measure your breathing at its worst and then give you inhaled medication to see if we can improve it.
If you are unable to stop your inhaled medication, we will be unable to complete all the tests to reach a diagnosis.
If you are attending the CDC for a test, you can expect any of the following:
Spirometry
Spirometry consists of a breathing technique from completely full lungs emptying all the way down. You may be asked to do this at different speeds.
Firstly, we will ask you to breathe normally through a mouthpiece and then take in as big a breath as you can. When we see that your lungs are completely full, we will then ask you to either blow the air out like a sigh or blast the air out as quickly as you can until your lungs are empty. Once they are empty, we will ask you to breathe back in as fast as possible until your lungs are full.
During the fast test it is important that the initial blast is as sharp as possible. You will be required to repeat the test for accuracy purposes.
Reversibility with Salbutamol
You may also be asked to perform the spirometry test again 20 minutes after being given inhaled medication. The aim is to see whether the medication has had a beneficial impact on your lung function results.
If you have any concerns about doing this or stopping your inhaled medication, please contact the department.
Please bring your inhaled medication so we can review it, and if necessary, you can take after the test is complete.
Exhaled nitric oxide test
This test involves breathing into a tube on a small handheld device. First you will be asked to blow out into the room and then take a big breath in on the tube. Once your lungs are full, we will ask you to blow down the tube at a set speed for about 10 seconds. The device will measure how much inflammation is in your airways from markers in your exhaled breath.
Single breath gas transfer
For the single breath gas transfer test, you will be asked to breathe normally on the mouthpiece, with your lips creating a tight seal and a peg on your nose. You will then be instructed to blow all the air out of your lungs until they are completely empty. Then you will be asked to take a breath in until your lungs are as full as possible and hold your breath for up to 10 seconds. Finally, you will blow out until your lungs are empty, keeping your lips tight throughout.
After the test, your results will be reviewed by the Respiratory Healthcare Scientist and sent back to the referring clinician. You will also receive a copy of the letter in the post or on MyChart.
Transport/mobility
Transport to and from the hospital can only be provided if needed for medical reasons. Please contact your GP in the first instance to see if you are eligible for this.
If you are a Cambridgeshire or Peterborough resident and require transport, please phone the East of England Ambulance service NHS Trust on 0345 603 8117 to arrange transport. Or contact Cambridgeshire & Peterborough EMED Hospital Transport on 0300 777 555.
Please ensure that you have booked a Wait and Return journey – hospital transport will wait for you throughout the duration of your appointment. If you have not booked a wait and return, you will need to wait for your transport to come and collect you.
When travelling via hospital transport, please ensure that you bring your medication or additional supplies with you as you may need to wait longer than expected.
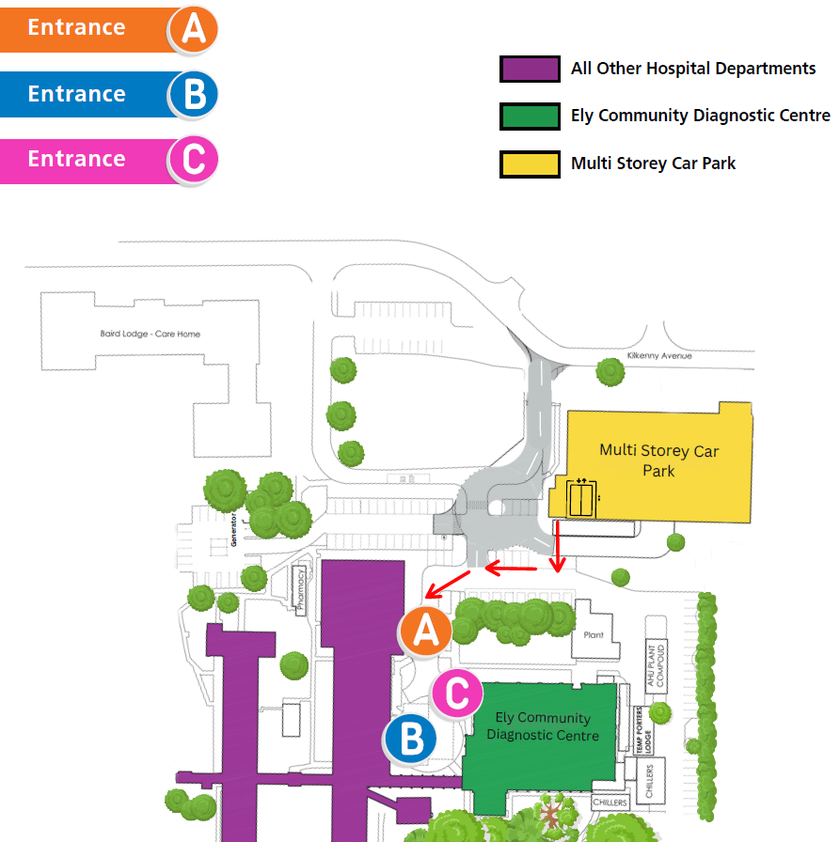
There is free parking available on site at the front of the hospital. Please see the map below.
What to do when you arrive
On arrival, please report to the Community Diagnostic Centre (CDC) reception area, where your registration details will be checked prior to your lung function tests.
This is located opposite the Docky Box Café at Entrance C. Please bring this letter with you on the day. There is limited seating available, however, you are welcome to bring along one relative or friend.
Directions to the Princess of Wales Hospital, Ely
You should put Davison Road in your sat-nav, rather than Lynn Road.
The full address is:
Ely Community Diagnostic Centre,
Entrance C,
Princess of Wales Hospital,
Lynn Road,
Ely,
CB6 1DN
MyChart:
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device.
More information is available on our website: MyChart
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

