Who is the leaflet is for? What is its aim?
This leaflet is designed to give general advice and information about the rehabilitation following trapeziectomy surgery to the thumb. This includes expected recovery time, hand therapy advice and exercises following surgery.
What is trapeziectomy surgery?
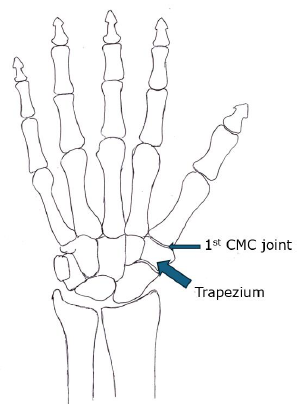
Trapeziectomy involves removal of the trapezium bone from the base of the thumb to stop the bone-to-bone arthritic pain that precedes the surgery.
A temporary k-wire can sometimes be used post-surgery for a few weeks to stabilise and maintain height of the thumb.
The final result of surgery can vary in each patient depending on the issues experienced prior to surgery. Most patients will experience a reduction in pain, improved movement and function, however surgery does not necessarily improve the strength in the thumb. You can discuss expected outcomes with your surgical team.
What does hand therapy involve after trapeziectomy?
Not all patients are referred to Hand Therapy following trapeziectomy surgery and this is at the discretion of the operating surgeon and/or consultant as to whether it is required.
If you are referred to Hand Therapy then the timing of your first appointment may vary depending how long the surgeon decides to keep your thumb and wrist immobilised post-surgery. Most patients are seen between 2-4 weeks post-surgery.
Hand Therapy aims to maximise the movement and function of your thumb/ hand, working within standard healing timeframes as well as your own individual recovery pace. Some patients can be fully functional within 3 months of surgery, however most patients find that strength, movement and function can take 6 months or more to fully recover.
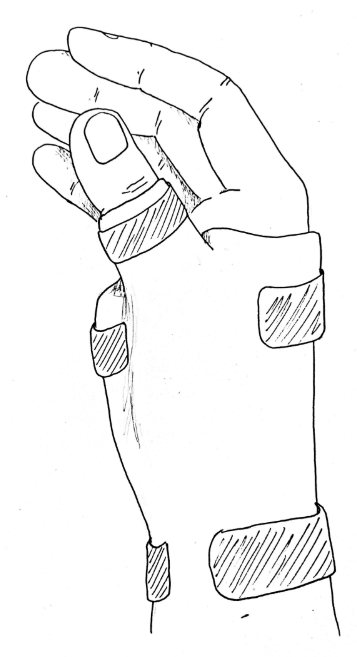
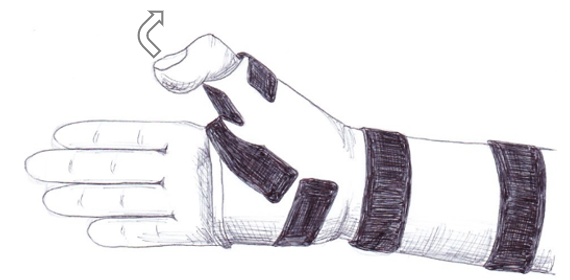
Splint
At your first Hand Therapy appointment a splint will be provided for you to wear. It may be pre-fabricated or custom-made depending on your needs and comfort. It is to be worn at all times except for hand hygiene and scar management (see below) for around four weeks post-surgery.
Check your skin regularly for red/pressure areas potentially caused by the splint and if the splint becomes too loose or too tight then please contact your hand therapist.
If it is a custom-made splint then make sure to keep it away from anything hot, such as a radiator, as this may cause it to change shape and fit to your hand.
Scar management
What is a scar?
Scars are collagen fibres produced as a result of the body’s normal healing process. The amount of scar tissue produced by the body varies depending on the individual and type of surgery/ injury.
Why is it important to care for your scar?
Initially scars can be firm, thick and red in colour (active phase) but over time soften and become pale in colour (matured). This whole process may take 12 to 18 months or more.
During the “active phase” you can use treatments to influence your scar. Initially as scar tissue forms it is firm and tacky and can stick to structures around it; scar care helps to flatten, make it softer and reduces the chance of scar tissue sticking (adhesions). Scar massage can be one of the most effect treatments to reduce scar tissue build up. The following section explains the technique.
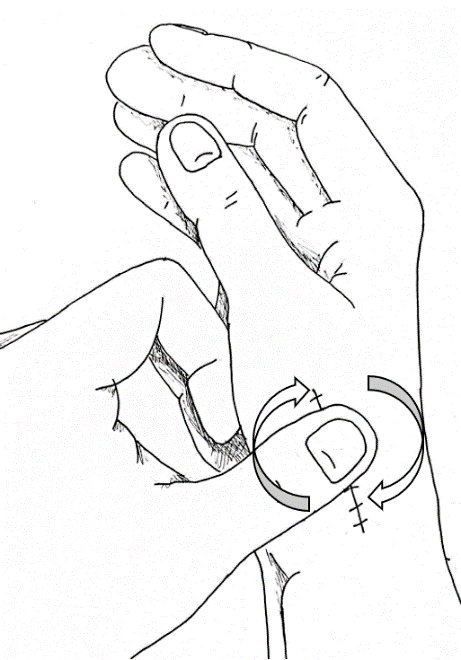
Manual scar massage
When can I start?
24-48hrs after your stitches have been removed, if the wound is dry.
If you have dissolvable stiches you start massaging your scar at approximately 12-14 days after your surgery, providing the wound is healed and dry.
What do I need?
You will need a basic, un-perfumed moisturising cream. For example aqueous cream or ‘E45 cream’ are ideal for massaging the scars.
Method
The scar massage needs to be in circular movements, on and around the scar line, to keep the skin moving freely. In the first few days you may only tolerate gentle massage but you should then aim to increase it to a deep and firm massage to reduce the risk of adhesions (see picture below).
Your therapist will advise you as to how long you should continue with your massage.
Start date………………………………..
Repeat ………..times per day for approximately……….minutes, ideally before your exercises.
Exercises
Exercise is important to benefit your recovery. It will reduce stiffness and swelling the hand and fingers and help to prevent complications.
For the first four weeks post-surgery, while wearing the splint, you will be advised to maintain the movement of the fingers and the thumb tip (see below) as well as free movement at your elbow and shoulder.
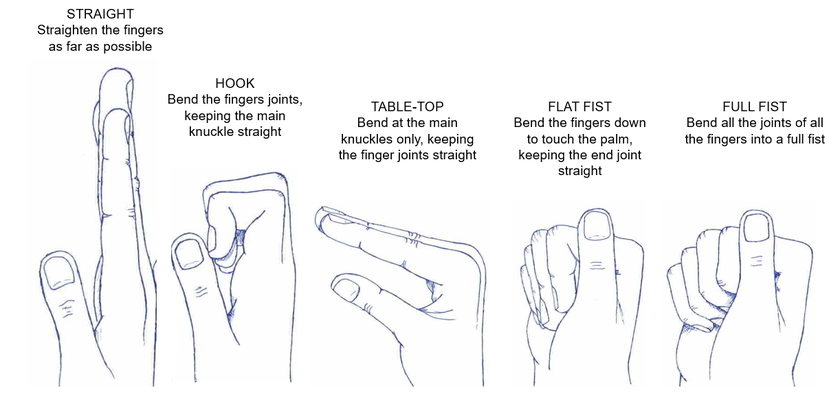
At four weeks post-surgery you will be advised on specific exercises to regain movement of the thumb. It will be stiff initially from being immobilised, but should loosen gradually with time and exercises.
Possible complications following surgery
Wound infection
If you suspect an infection it is important to contact your GP straight away. Signs of infection might include:
- Redness
- An increase in swelling
- A change in pain
- Discoloured discharge from a wound
- You may require antibiotics to treat the infection.
Swelling
It is normal to have some swelling present after surgery. This may remain in the hand or fingers for weeks to months. Swelling can change throughout the day. It is important to discuss concerns with your therapist, who will be able to advise you about the best course of action.
Pain
It is normal to experience some pain post-surgery. Each individual’s experience of pain is very different. The use of over-the-counter pain relief, as per the manufacturer’s instructions, can aid management of pain. If your whole hand is very painful and swollen post-surgery, it is advisable to contact your GP, therapist or consultant for advice.
What will be my recovery time frame following surgery?
When can I begin to use my hand?
Whilst you are wearing the splint (week 0-4 post-surgery) you will be advised not to use the thumb in function at all, however you can use the fingers for light tasks, using a scissor pinch.
After the initial 4 weeks, you can begin to use the thumb in function while wearing the splint, then out of the splint at 6 weeks, so long as your pain is well managed.
Sustained, heavy or repeated pinching to the thumb is avoided for 12 weeks post-surgery.
When can I drive?
This can depend on the extent of your operation and the pain you experience post-surgery. It is not advisable to drive while you are wearing a splint, therefore most patient resume driving around 4-8 weeks post-surgery, when they can confidently grip the steering wheel and control it if needed.
When can I wash my hand?
You can begin to wash the hand once the wound is fully closed or healed, usually after at least 7 days post-surgery. Initially it is advisable to wash it under running water rather than soaking it in water to avoid the risk of infection.
When can I return to work?
Returning to work will depend on the demands of your profession and the healing of your hand. In general, light manual work (e.g. office based) can usually be resumed while you are still in a splint at 2-4 weeks post-surgery, while heavier more manual work may be resumed at 10-12 weeks post-surgery. If possible, it is advised to return on lighter duties initially.
MyChart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device
More information is available on our website: MyChart
Contacts/further information
The Occupational Therapy department is located in clinic 30 in the Addenbrooke’s Treatment Centre (ATC). The Occupational Therapy reception telephone number is01223 216769.
References/sources of evidence
- Ataker et al (2012) Rehabilitation protocol after suspension arthroplasty of thumb carpometacarpal joint osteoarthritis, Journal of Hand Therapy, 25, p374-383.
- Henstridge, L. (2017) Development and implementation of a trapeziectomy rehabilitation protocol, Hand Therapy, 22(2), p64-72.
- Horlock & Belcher (2002) Early versus late mobilisation after simple excision of the trapezium, Journal of Bone and Joint Surgery, 84B(8), p1111-1115.
- Maqsood et al (2002) Interposition arthroplasty for osteoarthritis of trapezio metacarpal joint: results of a modified incision and technique of interposing with early mobilisation, Hand Surgery, 7(2), p201-206.
- Roberts et al (2001) Results following trapeziometacarpal arthroplasty of the thumb, Journal of Hand Therapy, 14, p202-207.
- Siegel et al (2022) Practice patterns following carpometacarpal (CMC) arthroplasty, Journal of Hand Therapy, 35, p67-73
- Wahon et al (2009) Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database of Systematic Reviews, Issue 4, DOI: 10.1002/14651858.CD004631.pub3.
- Wolfe et al (2014) A systematic review of postoperative hand therapy management of basal joint arthritis, Clinical Orthopaedics and Related Research, 472, p1190-1197
- Correspondence with all consultant surgeons at Cambridge University Hospital who regularly perform this operation.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

