Monitoring and Management of Heart Failure Symptoms
Introduction
Patients who have had a diagnosis of Heart Failure confirmed by a Cardiologist and have been referred to the Heart Failure Specialist Nurse (HFSN) team will be given this book.
This version of the book is for patients who are not under the care of GP Surgeries within the Addenbrookes Hospital Integrated HFSN team’s catchment area.
The aim of this book is to provide information regarding diagnosis, and to advise the patient how to recognise and manage symptoms related to Heart Failure.
This book is to ensure that patients have sufficient information to monitor and manage their symptoms until their local Heart Failure Specialist Nurse (HFSN) Team can review.
Who we are
We are the Addenbrooke's Integrated Nurse-Led Heart Failure Team.
We are a team of Specialist Cardiology Nurses, who help people diagnosed with Heart Failure to manage their symptoms and to stay well.
When you have been discharged home, we will refer you to your local HFSN service for ongoing Outpatient follow up.
What the Service Provides
The HFSN Service provides support in several different ways. Your local team will advise what is available from their service.
Normal heart function
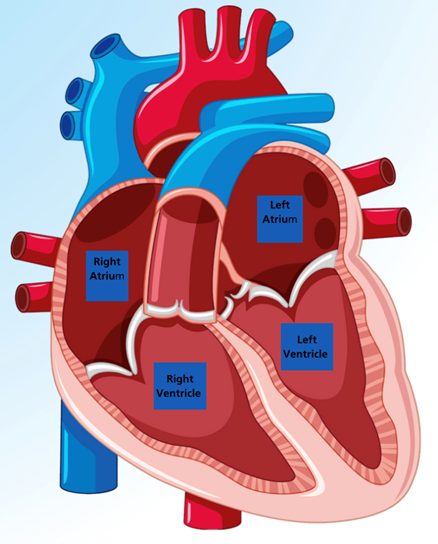
The heart is a pump made from muscle.
The heart is made from a special type of muscle that never gets tired in the way that other muscles do.
The heart pumps blood around the body via blood vessels.
Arteries (red) carry blood away from the heart to feed the body with oxygen and nutrients.
Veins (blue) carry blood back to the lungs to be refilled with oxygen.
The direction of blood flow in the heart is controlled by valves, which open to let blood through and close tightly to prevent blood going back the wrong way.
The heart has 4 chambers. The 2 large chambers at the bottom are called ventricles and are the main pumping chambers of the heart.
The 2 smaller chambers at the top are called atria and receive the blood from the blood vessels when the heart relaxes between pumps.
What is heart failure?
Heart failure is a chronic (long-term) condition, where the heart is no longer able to keep up with the demands of the body.
This means that the heart is no longer able to do its work properly without medical help.
Heart failure is diagnosed by your Cardiologist, using an investigation called a Transthoracic Echocardiogram (TTE or Echo).
Your cardiologist may order other investigations following your diagnosis to discover possible causes of Heart Failure.
The most common causes of Heart Failure are:
- Coronary Heart Disease, leading to the heart muscle becoming weak
- High blood pressure, leading to the heart muscle becoming stiff or thickened.
- Fluid overload caused by a narrowed valve or high blood pressure
- Rhythm problems, such as Atrial Fibrillation (AF), where the heart cannot beat in a coordinated manner.
- Heart Valve problems, either due to narrowed or leaky valves.
There are other rarer causes of Heart Failure, which your Cardiologist will discuss with you if needed.
Left Ventricular Function
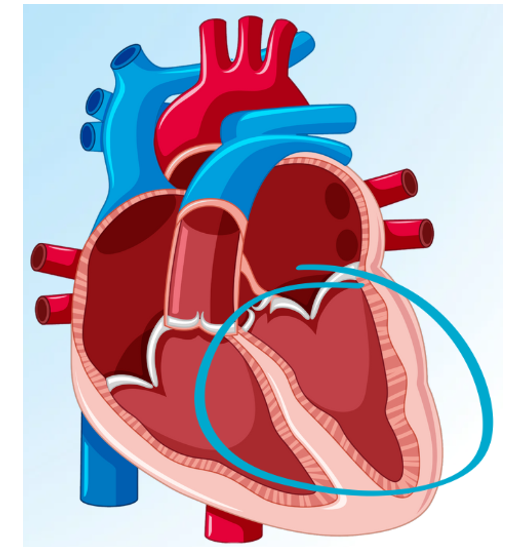
The pumping function of the ventricle is measured during the Echocardiogram.
Measurements of the blood in the chamber are taken before and after the heart pumps. In a normal heart, at least 50% of the blood in the left ventricle is pumped out. If the force of the beat is weaker, less blood is pumped out.
This is known as Left Ventricular Failure.
This measurement helps to classify Heart Failure into 4 groups:
Your diagnosis will be explained to you by your Cardiologist. They will also explain which classification of Heart Failure you have.
This helps to ensure that you get the right treatment to manage symptoms and help you stay well.
HErEF - Ejection Fraction less than 40% (Reduced Left Ventricular Function)
FHmEF - Ejection Fraction 40-49% (Moderately Reduced Left Ventricular Function)
HFpEF - Ejection Fraction 50% or more (Preserved Reduced Left Ventricular Function)
HFimpEF - Ejection Fraction, which has improved by at least 10%
Also known as HFrecEF
(Heart Failure with Recovered LV Function)
Managing Symptoms
When you have been discharged from hospital, we will send a referral to your local HFSN Service. They will make contact once they have accepted the referral. Until they have made their initial review, it is important that you monitor for any Heart Failure symptoms returning.
The main symptoms associated with Heart Failure are fatigue, breathlessness and swollen legs.
When the heart is unable to pump out as much blood as it used to, it causes a build-up of blood in the body. This is called Congestion.
Fatigue
When the heart is unable to pump properly, oxygen and nutrients are unable to get to the muscles. This leads to tiredness.
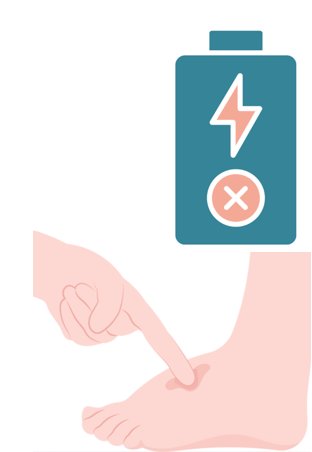
Oedema or Swelling
When the heart is unable to pump properly, blood tends to pool in the blood vessels. The extra pressure from this fluid causes the blood vessels to leak into the surrounding tissues.
If the fluid leaks into the tissues of the lungs, it can cause increased breathlessness or phlegm production. You may also notice a new productive cough.
If the fluid leaks into the tissues of the legs or abdomen, it causes swelling known as Dependent Oedema.
Regardless of where the fluid is stored, there will be an increase in body weight.
Breathlessness, wheezing or coughing
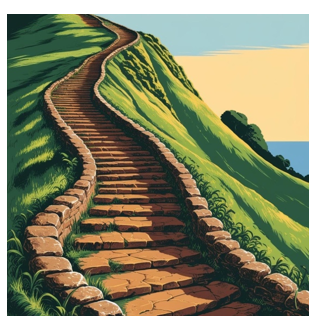
Build-up of fluid in the lungs takes up space where air would normally go. This leads to breathlessness, particularly when doing activities such as walking or climbing stairs.
Some people find they have trouble lying flat in bed and use extra pillows to help them breathe comfortably.
Breathing exercises can help too. They allow you to practise filling your lungs completely and making full use of your chest muscles.
Symptom monitoring and the NYHA Scale
The New York Heart Association Functional Classification (NHYA) is an easy way for doctors and nurses to measure how much symptoms are affecting your ability to perform day to day activities.
By using the NYHA scale yourself, you may be able to notice how well you are doing, or to notice when symptoms are increasing.
This will hopefully help you notice symptoms early and guide you to seeking advice and assistance.
NYHA Class 1 - I can perform all ordinary physical activities without getting overly short of breath or experiencing tiredness or palpitations.
NYHA Class 2 - I have slight limitation of physical activity. I get shortness of breath, tiredness or palpitations when performing more strenuous activity such as walking up a hill or climbing several flights of stairs. I remain comfortable at rest.
NYHA Class 3 - I have noticeable limitation of physical activity. I get shortness of Breath, tiredness or palpitations when performing activities less strenuous than ordinary activity. I remain comfortable at rest.
NYHA Class 4 - I am unable to carry out any physical activity without discomfort. I feel tired and short of breath even at rest. If any physical activity is undertaken, discomfort from my symptoms is increased.
Daily weights
Weighing yourself is an excellent way to monitor fluid levels. This measurement helps to monitor fluid levels in your body, as you are weighing your body, plus any extra fluid weight you may be carrying.
It is preferable to weigh yourself first thing in the morning, just after passing urine, and before eating breakfast.
You can record this weight on the table on the next page. Alternatively, some people have a notebook or even a spreadsheet.
If you notice a weight gain of 3-4 lbs (1-2kg) within 2 days which cannot be explained, or an unexpected slow, steady weight gain, this could be due to increased fluid in your body. Please phone our helpline to discuss this.
Alternatively contact your GP and tell them you have been diagnosed with Heart Failure. Tell them that you monitor your weights, have noticed a weight gain and tell them any new symptoms you may have noticed to gain their support or advice.
We don’t mind whether you use stones/pounds or kilograms.
As a guide, 1kg = 2.2lbs
| Date | Weight | Date | Weight | Date | Weight |
|---|---|---|---|---|---|
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
| Date | Weight | Date | Weight | Date | Weight |
Vital signs
We recommend that you check your blood pressure and heart rate regularly.
If you can, please consider buying a blood pressure monitor to use at home. You can buy one for £20-£30 either online or from your local pharmacy.
Alternatively, most GP surgeries and health centres have B/P measurement equipment. Pharmacies also offer B/P monitoring.
A blood pressure machine usually provides a heart rate but will not detect irregularities in your heart rhythm. It is much more accurate to take the pulse yourself.
Pulse oximeter machines are available online. Alternatively, you can find your own pulse and count how many times you feel it in one minute.
If your pulse feels irregular, it could be a sign of an irregular rhythm.
The most common irregular rhythm is Atrial Fibrillation (AF). This rhythm is more common over the age of 65.
If this rhythm is new, you should let your GP know
How to take a pulse
It is important to measure a resting heart rate, so sit and relax for 5 minutes before measuring.
Hold out your non-dominant hand with your palm facing upwards.
Press your index finger and middle finger of your other hand on the side of your wrist, just below the base of your thumb. Don’t use your thumb as it has its own pulse.
Press the skin lightly until you feel the pulse - if you can’t find it press a little more firmly or move the fingers slightly.
Once you find your pulse, count the beats you feel for 60 seconds.
A normal heart rate is between 60 and 100 beats per minute. If your heart rate is continuously above 120bpm or below 40bpm, we recommend you make an appointment to discuss this with your GP.

| Date | B/P | Pule | Date | B/P | Pule |
|---|---|---|---|---|---|
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
| Date | B/P | Pule | Date | B/P | Pule |
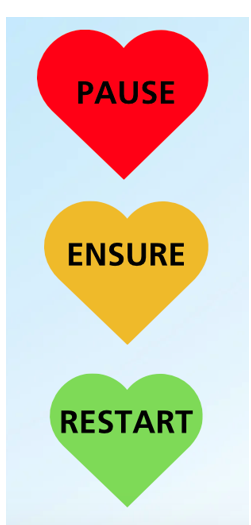
Sick day rules
Dapagliflozin - Potential Side Effects
Please contact your GP or HFSN straight away if you think you have any of the following side effects:
- Dehydration - You may notice a fast heart rate, have a very dry or sticky mouth or notice that you feel very thirsty. You may pass little or no urine and may feel very sleepy or tired.
- Soft Tissue Infection - This is a rare side effect. A serious infection of the soft tissue of the genital area can occur.
- Urine Infections (UTI’s) - Although urine infections are common, serious infections are rare. Signs of a UTI include pain or burning when passing urine, fever and/or chills, pain in your back or sides, or blood in the urine.
How to stay well




- Take care with how much fluid you drink. Advice will be given in clinic on what amount to try and aim for. If you are drinking more than 2 Litres (4 pints) of fluid per day, you are likely to be advised to reduce this. Milk with cereal or soup is not counted in your fluid intake.
- Alcohol - please try not to drink more than 14 units alcohol per week, as this can be harmful to your heart. If you need help, please speak with us or with your GP.
- If you are a smoker, it is of vital importance that you stop smoking. Support is available, please ask if you need support with this.
- Eat a healthy, balanced diet. If you are overweight, you will feel better if you lose weight. Advice on healthy eating is available if you require advice.
- If we advise you to reduce your salt intake, please try to as salt can make you hold onto fluids. Cooking with salt is fine but try not to season at the table. Please do not use salt substitutes such as Lo-Salt as this contains potassium. Please also try and avoid salty drinks such as Bovril or OXO. Also try and cook with reduced salt stock cubes or herbs and spices. Ready meals are often high in salt, so try and avoid these if possible.
- Exercise is of vital importance and has a huge effect on staying stable. Exercise will not harm you and can be increased safely. Exercise can even make you feel better by making you fitter overall. Always make sure to pace yourself and try not to rush. Cardiac rehabilitation is an excellent service to help increase exercise levels safely. Your HFSN or your GP will be happy to refer you if you would like to participate.
- Please ensure you have any immunisations you are offered, to protect you from potentially serious illnesses.
- Anxiety is common if you have heart problems. If you feel anxious, taking slow deep breaths can sometimes help. If anxiety is impacting your daily life, we can sign-post you to services that can help you. Alternatively, please speak with your GP.

- Please remember to weigh yourself every day
- If you can, please keep a record of your heart rate, blood pressure and weight so you can quickly spot any changes.
- Please keep a record of your medications.

- Please report any changes to symptoms, even if you are not feeling unwell.
- Please report any issues you may have with medications.
- Please report any changes you think may be due to your condition.
Getting more information
Heart Failure or Cardiology Resources
Pumping Marvellous (opens in a new tab) or 01772 796542
British Heart Foundation (opens in a new tab)
British Society for Heart Failure (opens in a new tab)
The Breathlessness Intervention Service or 01223 349325
Heart Failure Matters (opens in a new tab)
Medication Resources
Dapagliflozin (opens in a new tab)
Sacubitril/Valsartan (Entresto) (opens in a new tab)
Other Heart Failure Medications (opens in a new tab)
Older Adults Resources
Cambridgeshire County Council (opens in a new tab)
Non-Cardiology Resources
Psychological Wellbeing Service (IAPT) (opens in a new tab) or 0300 300 0055
Hospice UK (opens in a new tab) /Information and Support (opens in a new tab)
Sue Ryder palliative, neurological and bereavement support (opens in a new tab)
Arthur Rank Hospice (opens in a new tab) or 01223 675777
MyChart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device
More information is available on our website: MyChart
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

