Introduction
This information leaflet is for patients considering a Gastrostomy Tube. This may take place as a day case procedure or may require a short hospital admission. Your healthcare team will explain what is involved and answer any questions you may have.
Why do I need a gastrostomy tube?
You may have been given this leaflet after visiting our head and neck or thyroid oncology clinic, where we have recommended a gastrostomy tube as part of your care. This could be for the following reasons:.
- It is becoming more difficult for you to eat and drink
- We may have discussed that it’s not safe for you to eat and drink by mouth
- If you are having treatment, it may become more difficult for you to take food and drink by mouth
A gastrostomy tube can help as it bypasses the need to swallow, meaning nutrition and/or medications can be delivered directly into your stomach.
We understand you may have many questions about what this means, and this leaflet will provide answers to some of the more common questions that patients ask.
Can I still eat and drink?
Unless advised otherwise, you will be encouraged to continue eating and/or drinking as alongside the gastrostomy tube while having treatment. If you are finding it difficult to eat or drink due to the side effects of your treatment, your speech and language therapist and dietitian will advise and support you throughout your treatment. Please contact them if you have any concerns or questions.
If you have been advised that it is not safe for you to eat and drink by mouth, this will be discussed at length with you. If you decide to eat and drink despite this advice, we will support your decision and continue to offer you the same care. Deciding to continue to eat and drink will not prevent you from having a gastrostomy tube.
What is a Gastrostomy tube?
At Addenbrooke’s Hospital, PEXACT tubes are commonly used for Head and Neck patients. If your procedure is done at Peterborough you will most likely have a Freka tube inserted.
Both tubes are also known as a ‘PEG’, which stands for:
- Percutaneous (through the skin)
- Endoscopic (instrument used to examine the stomach)
- Gastrostomy (opening into the stomach)
What is a PEXACT gastrostomy tube?
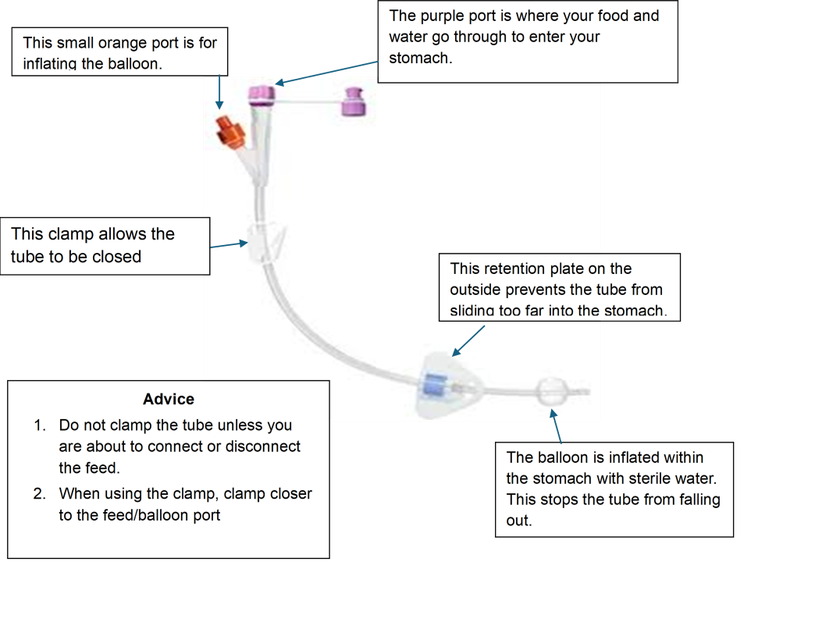
A PEXACT is a soft balloon retained feeding tube placed through your skin into your stomach to allow liquid feed, water and liquid medications to enter directly. This tube is held in place by a balloon filled with sterile water. It is important that the water in the balloon is changed weekly, and you will be shown how to do this by your Nutrition Nurse Specialist or local feed company Nurse.
Your feeding tube will look like this:
PEXACT Tube insertion
A gastroscope is inserted into your mouth passes through your throat and finally into your stomach. Alternatively, a nasal scope may be used which passes into your nostril, through your throat and finally into your stomach. This may cause you to gag slightly which is quite normal and will not interfere with your breathing. Your stomach will be inflated with some air so that we have a clear view to position. When the correct point is found in the stomach, two stitches are inserted to hold the stomach up against the abdominal wall, and then the tube is inserted from the outside.
The stitches will remain in place until the first tube change is carried out, usually four weeks after insertion. The tube is prevented from coming out of the stomach by a balloon which is inflated inside. The whole procedure usually takes 30 to 40 minutes.
You may feel a little bloated and have some wind-like pains because of the air in your gut; these usually settle down quickly.
What is a Freka PEG?
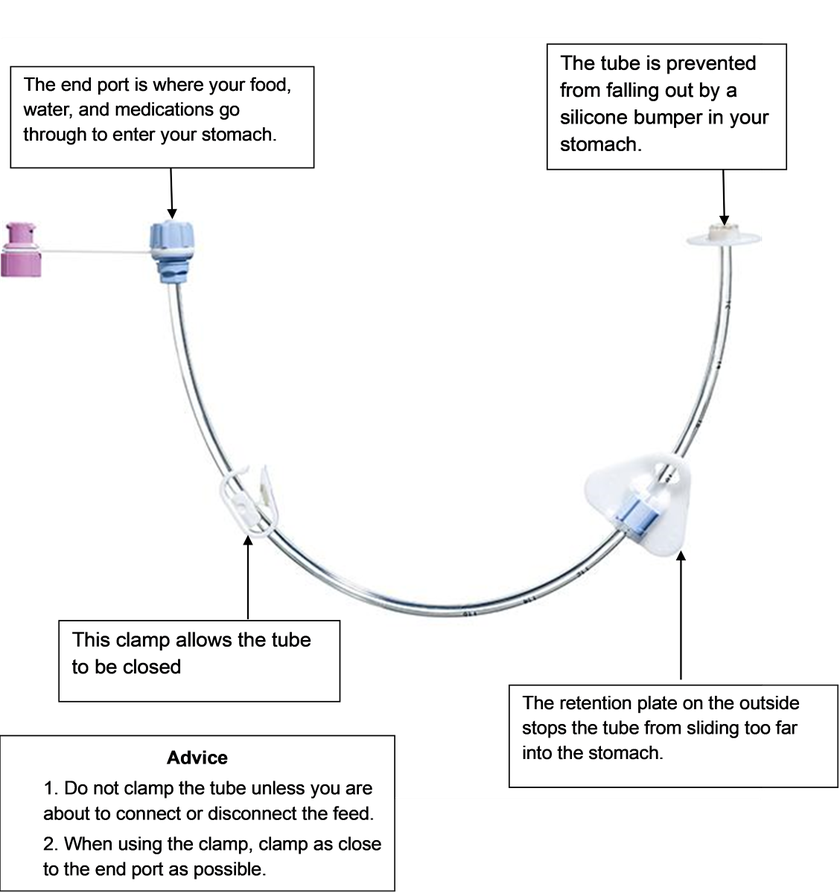
This is another type of soft feeding tube which also allows you to receive liquid food, water and sometimes liquid medicines directly into the stomach, but it is held in place by silicon disc (the ‘bumper’). You will be shown how to look after the tube by your nutrition nurse specialist or local feed company nurse.
Freka PEG insertion
A gastroscope is inserted into your mouth passes through your throat and finally into your stomach. This may cause you to gag slightly which is quite normal and will not interfere with your breathing. Your stomach will be inflated with some air so that we have a clear view to position
Once the endoscope is within the stomach, we pass a needle directly into the stomach. Using a small hole that we create from the outside, we place the gastrostomy tube and then secure it from the outside.
You may feel a little bloated and have some wind-like pains because of the air in your gut; these usually settle down quickly.
You will be supported by the team during the procedure however, if you make it clear that you are too uncomfortable the procedure will be stopped. The team can arrange a stop signal with you before starting the procedure
Your feeding tube will look like this

What are the risks of the procedure?
All patients being considered for PEG insertions are discussed at a weekly Feeding Issues Multidisciplinary team meeting to ensure this is an appropriate intervention. Additionally, the gastroenterology consultant will discuss the risk of the procedure with you when you attend for the procedure.
- Sedation: There is a small risk that sedation can relax the muscles needed for breathing. If we feel that sedation may be best avoided in your case we will consider placing it without sedation. We may even consider placing the tube using a nasal endoscope, which is safest and often the best tolerated approach.
- Aspiration: There are some risks associated with the endoscopic examination of the stomach when placing the tube, which could lead to aspiration and may cause pneumonia.
- Bleeding: while inserting the tube, there is a small risk of internal bleeding or puncturing an organ.
- Infection: after the procedure there is a small risk of infection within the abdomen (peritonitis), which is rare but can be serious.
- Death: Severe complications arising from the insertion of the tube are very rare. The risk of dying after the procedure is extremely low. Where deaths have occurred in our practice within the following 30 days of tube insertion they have been due to the underlying disease process rather than the procedure to place the tube itself.
You will be given a single dose of the broad-spectrum intravenous antibiotic called Gentamicin immediately after the procedure to minimise this risk. Gentamicin is safe to use in patients with penicillin allergy.
If you suffer with an allergy to Gentamicin or suffer with myasthenia gravis, Co-amoxiclav will be the alternative used.
Please note: For patients having PEG procedure at Addenbrooke’s Hospital
- You will be required to stay in the Endoscopy recovery area for four (4) hours where you will be closely monitored and 50mls of sterile water will be given through the PEG before you are discharged.
- If any strong (opioid) analgesia is given during the recovery period, you will need to be collected upon discharge as you will not be able to drive.
Important Notice: All PEGS placed at Addenbrooke’s Hospital
If you are discharged within 72 hours of having your PEG placed and you notice any of the following symptoms. DO NOT PUT anything through the PEG. Contact your GP (in working hours), Call 111 for advice or go to your nearest Accident and Emergency Urgently.
For tubes placed at Peterborough City Hospital: 01733 678433
Out of hours – please contact your GP - If you cannot wait to be seen by your GP, contact your local hospital’s emergency department.
PEG insertion After Care
There will be some discomfort after a gastrostomy insertion. However, if any of the following occur after the procedure, you must immediately stop feed or medicine delivery through the tube and contact your local Feed Company Nurse (please see contact details below)
- leakage of fluid around the tube
- pain on feeding or flushing your tube
- new bleeding
- redness
- yellow and smelly discharge
You will be trained in all the necessary techniques to look after the tube and what to do if you do have problems. Your dietitian or nutrition team will provide regular follow up, and the company delivering your feed will have a nurse helpline; details will be provided before you go home.
What problems might I encounter after placement of a gastrostomy tube?
Pain
The site where the tube enters the stomach can be painful for a few days after the procedure. Patients are usually encouraged to use pain killers (analgesia) regularly for the first two to three days following insertion. This will be discussed with you on the day of your procedure and painkillers prescribed if required.
Infection at the site of insertion:
This can occur if the PEG site is not kept clean and dry but is rarely serious. You will be provided with a PEG treatment kit containing Octenisan antimicrobial wash and Mupirocin antimicrobial ointment to clean the PEG insertion site for the first seven days. After this period patients are usually encouraged to clean with soap and water then dry well. Dressings are not usually required.
Leakage around the gastrostomy site
Occasionally feed or gastric (stomach) fluid may leak around the tube – this commonly occurs if the triangle plate or circular disc is not close to the skin allowing the tube to slide in and out of the stomach causing leakage. This can be corrected by tightening the retention plate (external bumper) close to the skin. The surrounding skin should be cleaned and kept dry. A protective skin barrier spray maybe applied to resolve any redness/ skin irritation caused by the leakage. In exceptional circumstances, the tube may need to be replaced, or repositioned at a different site.
Over granulation at the gastrostomy site
This is the appearance of light red or deep pink flesh that forms beyond the surface of the stoma opening. There are many reasons this may develop, and the treatment plans will be patient ‑specific.
PEG tube related problems
- Blockage of the tube: This can usually occur after giving some medications or not flushing the tube at the end of a feed. Though blockages can be resolved, you are encouraged to prevent this by flushing before and immediately after feed. Additional advice will be provided if you will be giving medications down the PEG tube.
- Balloon failure (burst balloon) If the balloon that retains your gastrostomy tube bursts the tube falls out. You will be required to attend your nearest Accident and Emergency department within an hour of your tube falling out to prevent the stoma (hole) from closing.
If the tube remains in place but balloon malfunction is suspected, you should secure the external triangle or round disc with tape to your abdomen to prevent the tube falling out before contacting your nutrition nurse for advice.
Feed related problems: diarrhoea or constipation. Your dietitian will advise on how to deal with these issues if they arise.
How long will I need to stay in hospital to have a gastrostomy tube placed?
Gastrostomy insertion is usually performed as a day-case procedure in the Endoscopy Unit. You will be required to stay in the Endoscopy recovery area for four (4) hours where you will be closely monitored. The nutrition nurses will teach you and/or your family how to look after the feeding tube if you have not had pre-insertion training. The PEG will be flushed before you are discharged.
What do I do if I have problems?
You will be trained in all the necessary techniques to look after the tube and what to do if you do have problems. Your dietitian or nutrition team will provide regular follow up and the company delivering your feed will have a nurse helpline; details will be provided before you go home.
How is the feed given?
When feed is required your dietitian will discuss the options available with you so that you can decide which is best for you. Feed will not be delivered until this discussion has taken place, and we will arrange all prescriptions and deliveries (or with your local Dietitians if needed). The nutrition nurse specialists may also be involved in this discussion to ensure you receive the correct equipment and training.
Feed and extra water may be given by syringe (bolus), or using a feeding pump during the day or overnight depending on your preference. All equipment and feed required will be provided (delivered) direct to you at no cost by your local feeding company.
Feeding can usually managed by the patient or relative. If this is not possible, special arrangements will need to be made before discharge from hospital. If you have concerns about how you will manage please let us know.
What nutrition (feed) is put through the tube?
Your Dietitian will discuss specialised liquid food (feed) that is designed to provide your body with the nutrients (carbohydrates, protein, fats, minerals and vitamins) that your body needs. They will also create a plan for you that will explain how much feed you need and when to have it. It is strongly recommended that only prescribed/approved feed, fluid and liquid medications are put through the tube to avoid damage and blockages.
How long will my tube last for?
Your first tube change will usually be completed by the Nutrition Nurse in hospital after four weeks, at which time your stitches will be removed. An appointment for this will be arranged for you here at Addenbrooke’s to attend the nutrition nurses’ clinic. After this, we usually recommend a routine tube replacement every four to six months and this can be changed at home by your local nutrition or feeding company nurse.
Freka PEG tubes that are well cared for can last for up to five years. One way of increasing the life of your tube is to leave the clamp undone when the end connector is in place. This prevents the clamp squashing the tube. You can also change the place the clamp closed along the tube to avoid pinching the same part of the tube each time. If no longer needed you will need to attend the hospital where your Freka PEG was placed for removal.
If you are having treatment, after it has finished, your dietitian and speech and language therapist will work with you to help you get back to you usual eating and drinking as soon as possible. Once you have not used your tube for feed, fluid or medications and your weight is stable for a minimum of one month, your doctor will discuss removing it. If your doctor is happy for your tube to be removed this will be done in hospital (Freka PEG) or at home (Pexact PEG) – your Dietitian will advise you which.
If you have a gastrostomy tube placed and decide that you no longer want it, please discuss with the Dietitians. We will check that you fully understand the risks of removing the tube, but will fully support your decision.
What if I decide not to have a feeding tube?
Again, we will check that you fully understand the risks of not having a tube, but will support your decision.
If you change your mind during treatment, and have made the decision to have a feeding tube because you are find eating and drinking difficult, it may be possible to insert a short term feeding tube called a nasogastric tube. Training for the tube and feeding pump (if required) can be done as an outpatient but this will be assessed on an individual basis. If you are unwell and require monitoring, admission will usually be advised and the team (doctor, dietician or SLT) will explain this to you.
It is not usually possible to place a gastrostomy tube during treatment.
If you are having treatment, deciding not to have a tube will not affect any treatment decisions. However, not having a tube means you are more likely to be admitted during treatment if you are struggling to eat and drink enough.
If you are finding it difficult to eat and drink because of your cancer, but decide not to have a feeding tube we will again support your decision. Your speech and language therapist and dietitian will continue to work with you to help you make the most of eating and drinking, and to make it as easy as possible, for as long as you find this helpful.
Pros and cons of gastrostomy tube placement
This is not an exhaustive list, but represents common issues our patients discuss with us. There is no ‘right or wrong’ decision, just what you feel is best for you. Please feel free to contact us with any questions or concerns you may have.
| Pros | Cons |
|---|---|
|
Pros
Can reduce stress and anxiety related to difficulty eating and drinking during treatment. |
Cons
Some people report less incentive to return to their usual eating habits after treatment. |
|
Pros
Can help support oral eating and drinking by making it easier to take pain relief and fluids. |
Cons
Invasive procedure, which can require overnight hospital admission. |
|
Pros
Can help to reduce the amount of weight lost during treatment, which can improve the likelihood of successful treatment. |
Cons
Some people find the tube difficult or unpleasant to manage. |
|
Pros
Can reduce stress and anxiety related to difficulty eating and drinking due to cancer. |
Cons |
What do patients who had a gastrostomy tube say?
'As much as I hated the thought of having a PEG tube, it was the right thing for me. By week 3 of my treatment, I couldn't tolerate food orally, it was easy to use the tube myself and for my family to administer it for me when I was too poorly to do it. I still lost weight but nutrition through the tube has kept it stable. I got used to the cleaning routine easily and there is always support when you need it. I will soon be having mine removed which I am so excited about but I will always be grateful that Peggy was there for me'.
‘When I was asked which I prefer to have a PEG or NGT...Without any hesitation, I choose PEG because of its convenience and easy access, I felt more confident to have it, no discomfort and manageable. It made my recovery faster and helped me a lot during the period that I struggle to swallow’.
‘For me having a PG has literally been a life saver. If your doctor suggests having a PEG fitted then just go for it. It guarantees you have excellent nutrition which is necessary for recovery and good health. You only realise you have one only when you use it for feeding and you will have training and support throughout’.
‘I was very sceptical at first and really didn’t want to have a PEG fitted but relented. It was done under local anaesthetic (not the best idea!) and I hated it from the moment it was fitted. But without it I wouldn’t be here today. It literally saved my life when I couldn’t eat by mouth for over 6 weeks’.
For further information from the patient’s perspective please see:
PINNT: A Support Group for People Receiving At Home Artificial Nutrition
Who to contact about what?
Addenbrooke’s covers many different areas and feed companies, and who to contact may be different at different stages of your care. If you are not clear who to contact please ask.
1. If you have any concerns about your feed or plastics order (including syringes and dressings) – contact your feed company:
Nutricia Homeward 0800 093 3674
Abbott Hospital to Home 0800 0183799
Fresenius Kabi 0808 100 1990
2. If you have any concerns about your feeding pump – contact your feed company:
Nutricia: 08457 623672
Abbott: 0800 0183799
Fresenius Kabi: 0808 100 1990
3. If you have any concerns about your PEG site or PEG tube contact:
For PEGs placed at Addenbrookes: 01223 216037 Option 1
For PEGs placed at Peterborough City Hospital: 01733 678433
4. Contact your Dietitian:
Phone: 01223 216655 Email: hn.dietitians@nhs.net
If you have any concerns about:
- any symptoms that suggest you are not tolerating your feed e.g. bloating, nausea
- your weight
- the amount or type of feed you take
- or if you need extra syringes or other supplies ordering
- or you want to discuss tube removal
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

