Your doctor has informed you that you have an epiretinal membrane.
What is an Epiretinal Membrane and what does this mean to you?
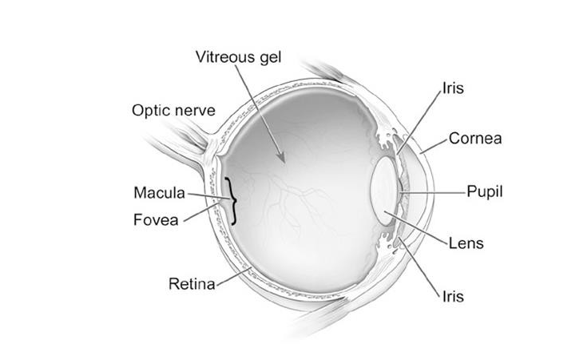
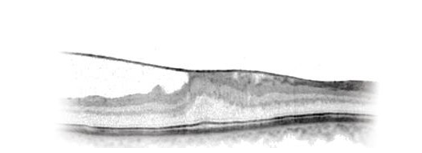
An Epiretinal Membrane (ERM) is a condition where a very thin layer of scar tissue forms on the surface of the retina, where the vision is sharpest. The part of the eye affected by the Epiretinal Membrane is called the macula, which is made of nerve cells and provides the sharp central vision needed for seeing fine detail (reading and driving for example). When an Epiretinal Membrane forms over the macula, it may contract and crumple over the macula resulting in distorted and/or blurred vision.
Why do I have an Epiretinal Membrane?
In most cases the development of an Epiretinal Membrane appears to be related to normal ageing changes inside the eye. In some cases it can be related to other conditions such as diabetes, blockage of blood vessel, inflammation or following retinal detachment. Epiretinal membranes are not related to macular degeneration. Epiretinal membranes in one eye do not usually affect the other eye. They are quite common, affect up to 8% of people over the age of 50, and can occur after retinal detachment surgery.

Assessment for Epiretinal Membrane
We are able to detect an Epiretinal Membrane during an eye examination following the use of eye drops that temporarily make your pupils large. Sometimes, a special scan of the back of the eye may be needed to confirm the presence of an Epiretinal Membrane. Your eye doctor will assess your symptoms to help you decide whether to proceed with surgery.
What should I expect with a diagnosis of Epiretinal Membrane?
In many cases, the discovery of an Epiretinal Membrane is by chance at a routine examination and the vision may not be affected. These Epiretinal Membranes tend not to change and do not always affect vision but then can occasionally get worse, causing blurring and/or distortion of vision. Treatment for Epiretinal Membrane is only required in those cases where the vision has been affected.
Epiretinal Membrane Removal
If an Epiretinal Membrane affects vision, the only way to treat it is to remove the membrane surgically. This is achieved by an operation called a vitrectomy, where specialised instruments are used to remove the jelly-like substance that normally fills the centre of the eye, called the vitreous. The removal of the vitreous inside the eye does not cause any permanent harm, apart from speeding up the development of a cataract. The vitreous is replaced by natural fluid produced inside the eye. In some cases, we will place a gas bubble inside your eye; the gas disappears on its own after a few weeks. Air travel is not permitted until the gas bubble has completely disappeared.
The operation for Epiretinal Membrane removal does not usually take longer than an hour and it can be performed either under a general anaesthetic or by using a local anaesthetic injection with the patient remaining comfortable and awake during the procedure. It is very important for the patient to stay still, especially during the very delicate manoeuvres when the membrane is removed using fine forceps.
Following membrane removal, the vision is typically more blurred and it can take months for it to improve. The operation is usually successful in reducing the distortion in vision due to an Epiretinal Membrane. If the vision had not been distorted prior to Epiretinal Membrane removal, improvement in the sharpness of vision and reading is less predictable.
What are the potential complications of epiretinal membrane removal?
As with any procedure there may be risks involved and you should discuss these fully with the surgical team prior to your operation. In a small minority, the vision may end up worse than before the surgery, and there is even a minimal chance of total loss of sight. Specific complications of Epiretinal Membrane removal include:
- Cataract - this means that the natural lens in eye has gone cloudy. If you have not already had a cataract operation, you will almost certainly get a cataract after the surgery. Your surgeon may offer combined surgery, with cataract extraction at the same time as the vitrectomy and Epiretinal Membrane peel.
- Retinal Detachment - the retina detaches from the back of the eye in 1-2% of patients undergoing vitrectomy surgery. The majority of retinal detachments are repairable, but further surgery is required.
- Bleeding - this is rare, but severe bleeding can result in vision loss.
- Infection - this is very rare and would be expected to occur in about 1 in 1000 patients, but needs urgent treatment and can lead to blindness.
- Raised eye pressure - an increase in pressure within the eye is quite common after surgery. In most cases it is short- lived and controlled with extra eye drops and tablets to reduce the pressure. If the high pressure is extreme or becomes prolonged, it may cause some damage to the optic nerve as a consequence.
What should I do following surgery?
Following surgery, you will be given eye drops to use for a few weeks, which will help the eye settle from surgery. The operation is usually performed as day case surgery. If an in-patient stay is required typically this would only be for one night. Patients are reviewed in clinic two to three weeks after surgery. In some cases, you may be asked to position your head in a certain way for some part of the day for a number of days. Otherwise, you can do most daily activities although you should avoid unhygienic environments and anything that puts the eye at risk of injury.
How much time off work will I need?
Most people will need at least two weeks off work after surgery. The amount of time off work will depend on the kind of work you do and the kind of surgery that is done. This will need to be discussed with your surgeon.
Medication
Bring all of your medicines (including inhalers, injections, creams, eye drops or patches) and a current repeat prescription from your GP
Please tell the ward staff about all of the medicines you use. During your stay If you wish to take your medication yourself (self-medicate) please speak with your nurse. Pharmacists visit the wards regularly and can help with any medicine queries.
My Chart
We would encourage you to sign up for MyChart. This is the electronic patient portal at Cambridge University Hospitals that enables patients to securely access parts of their health record held within the hospital’s electronic patient record system (Epic). It is available via your home computer or mobile device
More information is available on our My Chart pages.
Further information
The RNIB
- Helpline: 0303 123 9999
- Website: RNIB (opens in a new tab)
- Email: helpline@rnib.org.uk
The Macular Disease Society
- Helpline: 0845 241 2041
- Website: Macular Disease (opens in a new tab)
- Email: info@maculardisease.org
Scientific Evidence
The advice in this booklet is based on a variety of sources, including the latest research published in peer-reviewed scientific journals and guidance from the Britain & Eire Association of Vitreoretinal Surgeons (“BEAVRS”). If you require further information about this, please ask your ophthalmologist.
Contact details
Retinal Nurses (Monday–Friday 8am–5pm) 01223 274865
Privacy and dignity
Same sex bays and bathrooms are offered in all wards except critical care and theatre recovery areas where the use of high-tech equipment and/or specialist one to one care is required.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

