What does the gallbladder do?
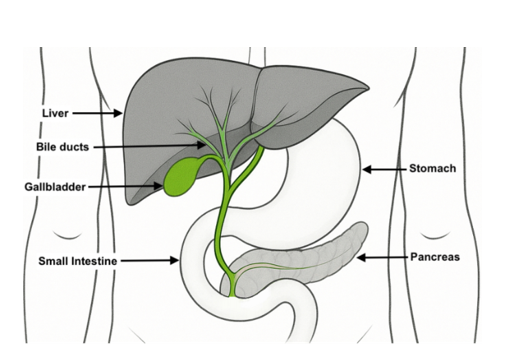
The gallbladder is a small, pear-shaped organ located under your liver. It stores, concentrates and releases bile. Bile is a digestive liquid made by the liver.
When we eat, bile is released from the gallbladder into the small intestine. Bile helps to digest and absorb the fat and fat-soluble vitamins that we eat and drink.
What are gallstones?
Gallstones are small hard stones that can sometimes form in the gallbladder. Most gallstones are composed of cholesterol, but they can also be formed of bile pigments or calcium deposits. Cholesterol precipitates or hardens into stones when the gallbladder empties less often than it should, or bile can become supersaturated with cholesterol.
Gallstones are more common as you get older. Obesity, rapid weight loss, and pregnancy also increase the risk of developing gallstones.
Complications of gallstones
Gallstones can block the flow of bile and can cause complications such as inflammation or infection in the gallbladder, bile ducts, pancreas or liver. Gallstones often do not cause symptoms. However, if a gallstone blocks one of the bile ducts, it can cause acute abdominal pain, discomfort or nausea and vomiting.
Do I need to follow a special diet?
You may have been advised to follow a low-fat diet to help manage symptoms. However, this is not the case for all patients, and there is little evidence to support this. Removing fats from your diet can also result in rapid weight loss and/or nutritional deficiencies. It is therefore recommended that you follow a healthy varied diet in line with the ‘Eatwell Guide’, including moderate amount(s) of fats as it is an essential component of a balanced diet.
Eatwell Guide
The Eatwell Guide provides a balanced framework for a healthy diet to help manage symptoms and reduce/prevent complications in gallbladder disease/gallstones.
The Eatwell Guide is divided into 5 main food groups, and it shows you how much of each section you should eat to achieve a healthy and balanced diet.

Aim to achieve this balance over a whole day or a week:
- Eat at least five portions of fruit and vegetables a day
- Base your meals around starchy carbohydrates, choosing wholegrains whenever you can e.g. bread, rice, potatoes, pasta and other starchy foods
- Include a variety of sources of protein: beans, pulses, tofu, fish, eggs, lean meats and other plant-based sources
- Have some dairy or dairy alternatives, opt for lower fat and lower sugar versions where possible
- Choose unsaturated oils and spreads and use sparingly/eat in small amounts e.g. vegetable oils and spreads.
- Limit your intake of foods and drinks high in fat and/or sugar and salt, including deep-fried foods, pastries and pies, fried snacks.
- Drink plenty of non-alcoholic fluids – the government recommends 6-8 cups/glasses a day
- Intakes of foods that are high in trans fatty acids should be minimal, these include: pastries and pies, deep-fried foods, fried snacks e.g. Crisps)
For more information see: Eatwell-guide (opens in a new tab)
Additional tips to help manage symptoms
- Try to eat regular meals, as missing meals and fasting reduces gall bladder emptying which increases the risk of stones forming or enlarging.
- If eating large meals causes discomfort try reducing your food portions and eat more frequently, this may reduce your symptoms.
- Eat breakfast soon after you wake up, as cholesterol concentrations are highest in bile produced overnight.
- If you find there is a link between your fat intake and your symptoms, trial reducing your fat intake to see if this helps. Tips for eating less fat:
- Try buying low fat versions of foods e.g. foods labelled as ‘low fat’, ‘light’ or ‘diet’.
- Check food labels and choose foods that contain less than 3g of total fat per 100g. These foods are labelled as green in the ‘traffic light’ system on the labels.
- Try micro-waving, steaming, poaching, boiling or grilling instead of roasting or frying.
- Use oil and butter sparingly. Try using small amounts of oil sprays and low-fat spreads instead.
- Take the skin and visible fat off meat/poultry before cooking.
- If you find there are other particular foods that trigger your symptoms, you could trial avoiding these to see if this helps.
- If you have steatorrhoea (pale, yellow, orange or oily stools which may float or be foul smelling) speak with your doctor or dietitian, as you may need more advice to help you further alter your diet.
How can I reduce my risk of developing further gallstones?
- Following a balanced diet as outlined above is recommended.
- Have regular meals including breakfast.
- If you are overweight, gradual weight loss can reduce the risk of developing gallstones. However, rapid weight loss (greater than 2 lbs or 1kg per week) or yoyo dieting is not recommended, as it may increase the risk of gallstone formation.
- Physical activity and reducing the amount of time sitting (sedentary) are also important to reduce risk of gallstones. Current UK guidelines recommend 150 minutes a week of moderate intensity exercise. For example, fast-paced walking, dancing or jogging. You should do physical activity and muscle-strengthening activity, such as weight-lifting, swimming or hill walking at least 2 days a week.
What happens if I have my gallbladder removed (cholecystectomy)?
After a gallbladder removal (cholecystectomy), most people do not have any problems with their digestion as the gallbladder is not essential. The liver will produce the same level of bile. This will just pass continuously into the bowel rather than being stored between meals.
You do not need to follow a low-fat diet after gallbladder removal. There is no evidence to suggest this is needed. Following a healthy well-balanced diet is advisable.
If after having your gallbladder removed you develop symptoms of diarrhoea, please speak to your doctor so this can be investigated.
Additional support
If you are underweight, losing weight unintentionally or you feel that you need more tailored dietary advice, please speak to your dietitian or ask your doctor to refer you to one.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

