This leaflet is intended to give you, as the patient, and your family and carers, information about the reason for your bone graft and the types of bone graft available to you.
Dental implants are used to replace missing teeth. This leaflet explains bone grafting procedures undertaken to allow implant placement. It gives you, your family and carers an overview of the different options available, the potential risks and benefits, and provides information to help you consent to this procedure. Your clinician will explain to you what to do after the procedure. If, after reading the leaflet, you have any questions you should contact your dentist.
This leaflet should be read in conjunction with the dental Implants leaflet you received when you were put on the implant waiting list.
What is bone grafting?
Bone grafting is any technique used to increase the amount of bone that you have in your jaw to help the best positioning of your dental implant. In order to have an implant, you must have sufficient bone at the implant site. This in turn aids the restoration, appearance and maintenance of the implant.
A variety of methods are available for bone grafting. The choice depends on the amount of grafting required, the anatomy of the area that needs grafting and your own preference.
If minimal bone grafting is required, it can be carried out at the time of your implant placement. If more extensive grafting is required, it will be carried out at least four months before your implant placement.
There are four main types of bone grafting explained in this leaflet:
- Guided bone regeneration (augmentation).
- Block grafting.
- Bone expansion.
- Distraction osteogenesis.
What bone grafting materials are used?
Bone grafting materials may be taken from you or other human, animal or synthetic sources. The graft material creates a scaffold for your own bone to grow into. This process may take between four and twelve months.
The most commonly used material is Bio-Oss. This artificial bone comes from bovine (cattle) bone, which has been sterilised and treated to make it safe for use as a bone substitute in humans. This is sometimes used by itself, or more commonly, mixed with particles or blocks of your own bone.
Additionally, a membrane patch may be placed over the bone graft to protect it from unfavourable cells entering from your overlying gum. These membranes are either dissolvable or non-dissolvable. However, non-dissolvable membranes are rarely used and involve a small surgical operation for removal after six to eight weeks. Dissolvable membranes are usually used and are made from human, animal and synthetic sources.
The most commonly used membrane is Bio-Gide, which is dissolvable. This artificial membrane comes from porcine (pig) origin.
Your surgeon will explain to you which products could be used for your bone grafting procedure.
If you have any concerns about use of animal-based products, please discuss them with your surgeon as soon as possible.
After full healing of the bone graft, dental implant placement is usually straightforward.
What are the risks of bone grafting?
In normal healing you should expect:
- pain to be controlled with simple painkillers, for example, ibuprofen or paracetamol
- swelling to be at its worst after two days
- bruising over the face to appear
- to feel better after stitches are removed, after seven to ten days’ time
Problems that may occur straight away:
- swelling
- numbness from local anaesthetic
- pain
- bleeding: you may experience a nosebleed
Problems that may occur later:
- infection of the bone graft area
- graft exposure
- facial pain and swelling after two to seven days
- severe facial bruising appearing after one to three days
- no graft present after the completion of the healing phase. The risk of failure varies and is higher in some people, especially in smokers. Your surgeon will tell you if they think your risk of failure is higher than normal
- insufficient amount of your own bone generated for implant placement
Problems that are rare, but serious:
- long-term numbness/tingling/discomfort from lower jaw, cheek, chin, lip, and tongue
- an oro-antral fistula between the sinus and mouth which requires further surgery to close
- longer-term infection necessitating graft removal
Minor risks are expected in around 30% of cases. Severe risks are rarer.
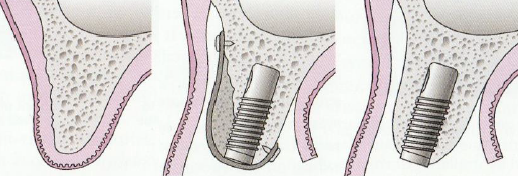
Guided bone regeneration
If any part of the implant is not covered by bone once in place, the technique of guided bone regeneration can be undertaken. It involves a small amount of bone harvested from around the site of the implant. The procedure is often carried out at the same time as implant placement and usually no extra healing time is required. The bone is placed over any exposed parts and is often mixed with another bone graft material, for example Bio-Oss. Following placement of the bone graft particles, the area is covered with a membrane patch, usually Bio-Gide. Stitches are inserted as normal and healing is usually uneventful.
Block grafting
This procedure is used where more extensive bone grafting is required. Bone to be grafted is provided by either a bone bank from other humans, or more commonly, from your own hip, jaw, chin, or scalp. These grafts are screwed into the bone in your mouth. These screws will be removed at the same time as your implant placement.
Bone grafts from the hip are the most common, as it is possible to harvest a considerable amount of suitable bone from this region. The hip bone will grow back after the graft. This method results in a scar of around 8cm along the pant line. Occasionally, grafts may need to be taken from both sides of the hip. This method results in some soreness and requires an overnight stay in hospital. After a hip graft, around four weeks of rest are required before you can exercise. You should be aware that there is a risk of permanent numbness over the site. In the hospital you will be given powerful painkillers to manage the pain; following discharge, oral painkillers should control any pain and discomfort. After three months the bone in the hip should have grown back. After four to six months the bone grafts will have healed and your dental implants can be placed.

An alternative to grafting from the hip is grafting taking bone from your scalp, where scarring is less obvious.
The other option is to graft from the jaw or chin. However, there is less bone available here, so taking bone from this area is only done when less grafting is required.
You should be aware that all of these options carry the additional risks of numbness to the lips and cheeks, drooping of the upper eyelid and the development of a dimple in the chin.
If block grafting is required, your dentist will discuss with you the best option and the details specific to your case.

Alternatives to block grafting
Bone expansion
This is also known as ridge splitting or an inter-positional graft. An alternative method to block grafting. Bone expansion is where the existing bone at the implant site is split and separated to create a gap in order to widen it. The space in the split is then filled with a bone graft, usually particles of your own bone mixed with Bio-Oss. However, this option is rarely undertaken as adequate length and width of bone are required for successful performance.
Distraction osteogenesis
This is a further alternative to block grafting. The method involves splitting the jawbone where the implant is planned, creating a gap, and attaching a metal device with a screw head left sticking out of the gum. The turning of this screw creates a gap to allow your own bone to grow and fill that gap. You will be required to turn the screw head every few days, which in turn moves part of the split bone away from the other part, while the area between the split heals with new bone. Once adequate bone has grown in the gap, the device will be surgically removed. Removal is followed by a period of healing before implants can be placed. This procedure is rarely undertaken as it involves a complex technique and can be cumbersome for you.
What alternatives are available to bone grafts?
The most common alternatives to bone grafting include:
Angled implants
Angled implants are used as an alternative in order to avoid simple bone grafting. When used, these have similar survival and success outcomes to conventional implants after five years. But if extensive bone grafting is required, angled implants rarely provide an alternative.
Zygomatic and pterygoid implants
These implants are placed into cheek and facial bones that lie behind the upper jaw. They are long and angled so that they are put into the mouth in the form of either removable dentures or fixed bridges. The surgery is more complicated than conventional dental implant placement.
Bridges fixed onto adjacent teeth
This procedure includes either gluing directly onto the adjacent tooth / teeth (adhesive resin-bonded bridges) or filing down the adjacent tooth/teeth for crowns (conventional bridges). The type of bridge used, depends on the length of the space, the quality of available tooth structure on the adjacent teeth, the bite, and the tooth nerve status. Usually, only one or two teeth can be replaced on a bridge.
Conventional bridges carry the risk of damaging the nerve in the filed tooth and may necessitate root canal treatment or extraction in between 5 and 19% of teeth. Resin-bonded bridges do not require tooth reduction and there is minimal risk of needing root canal treatment.
Dentures
If implants and bridges are not feasible in your case, your missing teeth can be replaced on a removable denture or ‘plate’. These need to be removed after eating for cleaning and left out overnight to avoid gum infections underneath the denture.
No tooth replacement
If there are sufficient functional teeth in the mouth it may be better to accept the space.
Contact details
Restorative Dentistry, Clinic 8, Box 47, Addenbrooke’s Hospital, Cambridge, CB2 0QQ
Opening hours: 09:00 (9am) to 17:00 (5pm) Monday to Friday.
Direct line: 01223 216412
Contact Centre: 01223 245151
How to find us

If you need any further information or have any concerns or worries before or after your procedure, please call Clinic 8 on 1223 216412.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

