Introduction
This information leaflet has been written for parents and carers of children for whom biofeedback therapy has been recommended. It explains what biofeedback therapy is, which children are suitable for biofeedback, what the therapy sessions involve and how to prepare your child for them.
At the end of this leaflet you will find contact numbers for use if you have further questions or queries.
What is biofeedback?
Biofeedback therapy is designed to help your child learn how to control a specific part of their body which they do not normally consciously think about. In children’s urology, biofeedback is used to teach the child how to retrain the pelvic floor muscles which are important in bladder function. During biofeedback a computer is used to measure, record and display feedback information about how the pelvic floor muscles are working. Over a number of sessions children can learn to contract (squeeze) and relax their muscles correctly and so improve their bladder and voiding (weeing) symptoms.

Where are the pelvic floor muscles?
Many children with urinary symptoms such as incontinence or incomplete bladder emptying have difficulty controlling the muscles used to void (wee). The pelvic floor muscles are at the base of the pelvis, below the bladder and are shaped like a sling. Both males and females have pelvic floor muscles.

If the muscles are weak the bladder may leak between voids. However, if the muscles are too tight there may be difficulty passing urine and the bladder may retain some urine rather than emptying completely.
By using biofeedback training, children can learn how to contract (squeeze) and relax their muscles correctly. The goal of biofeedback training is to improve your child’s ability to store urine and to empty his/her bladder more effectively.
Which children can benefit from biofeedback therapy?
Children can experience many different bladder and voiding problems and a separate leaflet is available on bladder and voiding problems in children; please ask if you would like one. Biofeedback therapy can help children who:
- Do not empty their bladder completely during voiding - If your child is unable to fully relax their muscles to void (wee) the bladder may not fully empty, which can lead to urinary tract infections and incontinence (‘wetting’). Biofeedback training teaches children to relax these muscles so in turn, improve their bladder emptying.
- Strain to void
- Void with a start-stop-start pattern
- Take a long time to void and have little ‘force’ in their urinary stream.
- Leak urine during coughing, sneezing or exercise - If your child has a weakened pelvic floor this can cause incontinence (leakage of urine) when the abdominal (tummy) pressure increases due to coughing, sneezing or during exercise.
Biofeedback teaches your child to identify the pelvic floor muscles and learn exercises to strengthen them. In order to understand and participate in biofeedback children usually need to be aged seven years or more; occasionally younger children (aged five or six years) may be mature enough to understand what to do.
What happens during biofeedback therapy?
Biofeedback therapy takes place over a number of sessions. The initial session is the longest and takes two to three hours. During the initial session your child will be shown the equipment and how it works and then will need some time to practice. Follow-up sessions are shorter; usually one hour in each duration.
At the beginning of every session the nurse specialist will ask you questions about your child’s voiding, drinking and stooling pattern, such as how:
- much water does your child drink
- often does your child pass urine
- often is your child wet between voids
- often does your child open their bowels and what does the stool (poo) look like
It can be useful to keep some notes about your child’s drinking and voiding and we can supply you with diaries for this purpose. Please ask if you would like one.
Biofeedback works by measuring and displaying pelvic floor muscle functions on a computer screen which have been picked up through electrode pads placed on the child’s body. The nurse will apply sticky electrode pads either side of your child’s anus (bottom), another set on the abdomen (‘tummy’) and a final set on the bony part of the hip. Below are photographs of the electrode pads used. The sticky pads are then connected to the computer using wires; which are long so your child can stay fully clothed whilst receiving biofeedback.

Once the electrodes are in place the computer will show us what the muscles are doing; either squeezing or relaxing. The information is then turned into pictures and sound on a TV screen.
By seeing and hearing these images your child will be able to understand exactly what their muscles are doing; if they change what their muscles are doing, the pictures and sound also change; this way your child learns to control their pelvic floor muscles.
The nurse will explain how to control an animated character on the computer screen (see example in photograph below). It can be quite difficult to work out which muscles to squeeze initially – the electrodes on the abdomen will help us see if your child is using these muscles rather than the pelvic floor muscles.

Bladder scan
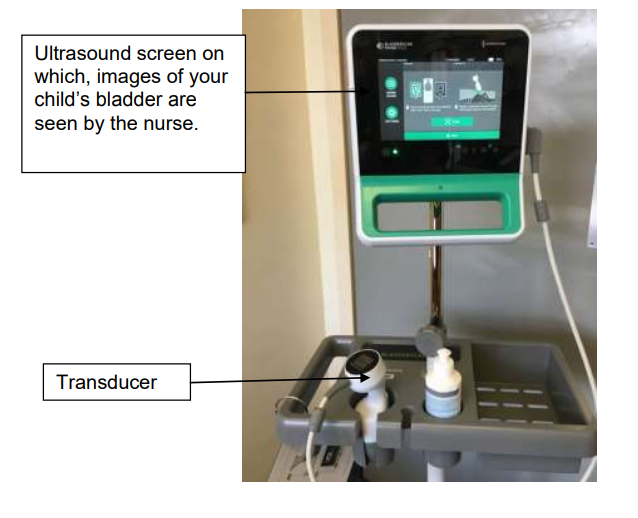
During the sessions the specialist nurse will also undertake a portable bladder scan to measure the volume of urine (wee) in your child’s bladder. The scan is a type of ultrasound. Gel is placed on your child’s lower abdomen over the bladder and then a transducer (see picture below) is passed over the lower abdomen so any urine in the bladder can be seen.
Uroflowmetry
During the biofeedback therapy your child’s urine flow rate will be measured as well. Uroflowmetry (also called a ‘flow rate test’) involves urinating into a machine which has the appearance of a portable toilet (see photograph below). The machine has a computer attached which measures how much urine your child passes and how quickly.

Is any part of the session painful?
Biofeedback therapy, ultrasound and uroflowmetry are not at all painful. Having the sticky pads peeled off at the end of the biofeedback session may be a little uncomfortable (similar to having a plaster removed).
How many sessions of biofeedback therapy will my child need?
Every child is different. Most children will need three or four sessions but some will need up to a maximum of six sessions to learn the proper methods and exercises to help relax and control pelvic floor muscles. Sessions are scheduled to take place every four to six weeks.
How to prepare for biofeedback sessions
- It is important that your child knows what to expect on the day. Your nurse specialist will help explain what will happen in language your child can understand and talking to your child at home and answering their questions is important. If you cannot answer your child’s questions write them down so they are not forgotten and your nurse specialist will be pleased to help answer them.
- Ensure your child knows that sticky pads will be put onto their body, that this will be undertaken in privacy by a trained nurse and that you will be with them.
- Ensure your child knows that biofeedback therapy and ultrasound are not painful at all.
- Your child should wear comfortable loose fitting clothes, such as track suit bottoms; if appropriate bring incontinence pads and a spare set of clothes.
- The first session can last for two hours so you may want to bring something to read or do.
- We are only able to provide drinking water; but there are facilities for patients to buy food and drink from.
What happens between biofeedback sessions and after they have finished?
Like all muscles, the pelvic floor muscles need regular exercising so continuing the exercises at home is essential The biofeedback sessions themselves are designed to teach your child how to locate and isolate the important muscles for voiding and each follow up session allows us to re-assess learning. It is the practice undertaken at home which exercises these muscles; the more practice undertaken at home the sooner symptoms will improve. Your nurse specialist will advise you of the exercises your child needs and how often to perform these but generally we advise that 5 minutes per day should be spent performing the exercises as a minimum.
What else can I do to help my child between biofeedback sessions and after they have finished?
- Ensuring your child drinks enough, drinks appropriate types of fluid and drinks frequently through the day are all important in maintaining bladder health. Full information is available in our leaflet, ‘bladder and voiding problems in children’; please ask if you would like a copy.
- Voiding regularly, voiding in an appropriate position and cleaning the genitalia appropriately are also important in maintaining bladder health. Full information is available in our leaflet mentioned above. Please ask if you would like a copy.
How successful is biofeedback therapy?
Research studies focussing on biofeedback in children suggest that over 50% of them may expect resolution of symptoms whilst others will have improved symptoms. Some children however will not benefit from biofeedback therapy.
A good amount of practice performed at home is important in achieving success.
Are there any risks with biofeedback?
There are no risks with biofeedback or the use of ultra sound and it causes no discomfort.
Are there alternatives to biofeedback?
There are other things you can do to aid bladder health which will have been discussed with you in clinic with your specialist nurse or doctor; these include
- drinking plenty (especially water)
- drinking regularly throughout the day
- avoiding carbonated and caffeinated drinks and also drinks that contain blackcurrants
- double voiding (passing urine then counting to 20 slowly before trying to pass urine again)
- preventing and treating constipation
How are sessions booked?
All biofeedback therapy sessions are coordinated and led by the children’s nurse specialists from the department of children’s urology. Prior to the initial session the nurse specialist will confirm that your child has undergone appropriate prior assessments with either one of the specialist nurses or doctors and has symptoms that biofeedback is likely to help.
One of the nurse specialists will telephone you to arrange a date and time for the initial session. Details of the appointment will then be confirmed by letter to you. At the end of each session the next one is booked with you by the nurse specialist.
Biofeedback therapy sessions are held in our children’s outpatient clinic.
What happens if I can’t attend a session or my child is unwell on the day of the session?
It is important that you can commit to attending a series of sessions of biofeedback. If an arranged date becomes inconvenient it is essential that you contact the nurse specialist team as soon as possible so that another date can be arranged for your child and another child can be offered the session that you are unable to attend.
It is important that your child is well on the day of the biofeedback session. If your child is unwell it is essential that you contact the nurse specialist team to discuss and rearrange.
Chaperoning
During your child’s hospital visits he/she may need to be examined to help diagnose and to plan care. This examination may take place before, during and after treatment, by trained members of staff and will always be explained to you beforehand. A chaperone is a separate member of staff who is present during the examination. The role of the chaperone is to provide practical assistance with the examination and to provide support to the child, family member/ carer and to the person examining.
Who shall I contact if I have any queries, concerns or questions?
For further information/queries please contact: Your nurse specialist (Monday to Friday 08:00 to 18:00)…01223 586973………………...
The ward/clinic you were on…………………………………………………………..
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

