This leaflet has been developed to provide an overview of Cancer Services at Cambridge University Hospitals NHS Foundation Trust (CUH) based on the Cambridge Biomedical Campus. The aim is to support you, your family and any carers during your cancer treatment. It contains information about some of our cancer wards, clinics and services across the campus, but this does not mean that you will see all these different areas and people. Your treatment will be specifically designed for your needs and therefore you will only see the areas and staff relevant to your treatment.
Included in this leaflet, you will find information about:
- Cancer inpatient and outpatient areas
- The Cancer Support Service including the Information Team and cancer navigators
- Your clinical nurse specialist
- Maggie’s Centre Cambridge
- Rehabilitation and Exercise during Addenbrooke’s Cancer Treatment (REACT)
- Patient Transport Services
- Parking for patients undergoing chemotherapy and radiotherapy
- Telephone and video appointments
- MyChart – electronic patient portal
- Cancer Research UK
- Patient Advice and Liaison Service (PALS)
- Carers and available support
- Information about the application for prescription charge exemption form
- Additional resources from Macmillan
Cancer services at CUH
More than 20,000 new patients are seen each year at CUH. It is a regional centre for rarer types of cancer and is also the local hospital for patients living in the Cambridge area. Adult cancer patients are seen across the CUH campus within all specialties and services. Treatment for children is managed by the Paediatric Haematology and Oncology department in the hospital.
An example of some of the Cancer Services at CUH include:
- The Department of Oncology - treats cancers of the solid organs, such as lungs or liver, using:
- Chemotherapy - which uses anti-cancer drugs to either destroy or control the growth of cancer cells and/or,
- Radiotherapy – which uses high energy radiation to treat a variety of cancers.
- The Department of Haematology - treats cancers of the blood, such as leukaemia, as well as non-cancerous blood disorders with a combination of oral chemotherapy and blood products.
- The Cambridge Breast Unit - offers a Breast Screening Service as well as providing referral clinics for patients with breast symptoms. The rapid diagnosis clinic for both, “symptomatic” and “screening”, aims for same day assessment encompassing consultation with a clinician and if needed, imaging and further investigation. The unit provides multi-disciplinary breast disease management including surgery.
- Gynaecological Oncology - The Gynaecological Oncology specialty provides cancer care focusing on the diagnosis and treatment of cancers affecting women's reproductive organs, such as the uterus.
- The Department of Urology - provides all diagnostics and treatments for both malignant and non-malignant urinary tract conditions.
- Cancer Support Service - a multi-disciplinary team provides advice and support for different cancers, financial support, emotional issues and a wide range of other challenges, as well as individualised support to fully address each patient's concerns.
- Palliative care - offers specialist advice and support both on symptom and total care of patients with life-limiting illness.
The provision of services to patients is closely linked with the:
- University of Cambridge Department of Oncology and Haematology, which ensures that high-quality cancer care is underpinned by research excellence,
- Cambridge Cancer Trials Centre (CCTC), which collaborates with external pharmaceutical companies to improve the outcome for patients with cancer, or at risk of developing cancer, by designing and conducting excellent clinical trials and studies,
- Cancer Research UK (CRUK) Cambridge Centre, which is the collaboration of scientists and clinicians from CUH NHS Foundation Trust, the University of Cambridge, independent research institutes, and pharmaceutical and biotechnology industries in the Cambridge area.
Visiting the hospital
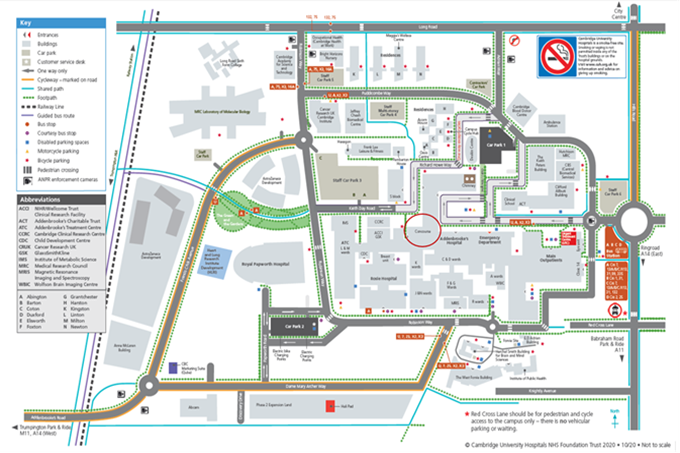
CUH is based on a large site, and you and your family may need to visit several areas of it. There is a free courtesy bus running every 30 minutes from car parks 1 and 2, which can drop and collect you from the main entrances.
The CUH Directions mobile app is also available for patients and visitors. It helps you to find your way around the Addenbrooke’s and Rosie hospitals, making it easier to locate clinics, wards and other facilities on our campus.
How to download CUH Directions
- Visit the App Store or Google Play Store on your mobile device
- Search for "CUH Directions"
- Download and install the app
- Launch the app and start using it to navigate our hospitals
The app can be downloaded on iOS and Android devices. After you have downloaded it, the CUH Directions can be used without any internet access (WiFi or data).
Oncology and haematology outpatient services
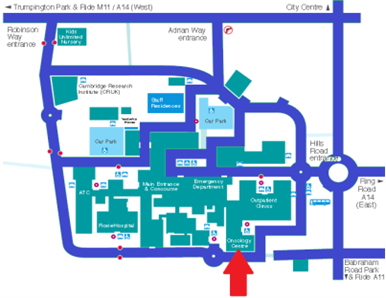
The main oncology and haematology services are located off the outpatient corridor on level 2, between the outpatient entrance and the main concourse area and can be approached from either direction. There is also a separate access off Robinson Way, via car park 2.
The Oncology and Haematology Outpatient area is home to the:
- Oncology and Haematology Clinic Suite - all Oncology and Haematology departments Outpatient clinics are held within the clinic suite. There are usually between six and seven clinics held each day, all of which are run by a team of nursing and medical staff supported by administrators. Normally, 28 sessions are held per week, seeing approximately 1000 patients.
- Radiotherapy Department - sees over 200 patients a day and offers a wide range of radiotherapy treatments to serve the local and regional population. The department has seven linear accelerators, treatment units, two dedicated CT scanners, an orthovoltage (a type of deep x-ray) unit and also offers an inpatient/outpatient brachytherapy (a form of radiotherapy) service.
- Oncology Day Unit and Chemotherapy Suite - provides care for people who are receiving their treatment as a day case.
- Cancer Assessment Unit - this unit cares for cancer patients needing urgent care due to a complication of their cancer or treatment.
- The Cancer Support Service Pod - The home of the Cancer Support Service at CUH providing patient support and wayfinding for the cancer pathway.
Haematology day unit
The Haematology Day Unit is located opposite the main hospital entrance. Approach the main entrance, but do not enter and instead follow round to the right at the end of the covered walkway from Car Park 1 - the entrance to the unit is in the corner (opposite the main entrance).
This area provides care for people, who are receiving treatment as a day case. It has been specially designed to care for haematology patients who require close outpatient review.
The East Anglia Blood and Marrow Transplant Unit is also located in Addenbrooke’s Hospital and provides a comprehensive service for the treatment of cancer using high-dose therapy with bone marrow, peripheral blood stem-cell support and CAR-T cell therapy.
Inpatient wards and apheresis
The Oncology and Haematology wards are located in the main ward block of Addenbrooke’s Hospital and can be accessed via the C and D lifts found off the main corridor and next to the hospital concourse.
Ward D9 - oncology unit
This ward provides care for all oncology patients undergoing inpatient chemotherapy treatment. It also provides care for people who are undergoing radiotherapy and need to
be in hospital for this or have a problem related to their illness or treatment.
Ward C10 - haematology and BMT unit
This area provides a comprehensive service for the treatment of haematological diseases (cancer and non-cancer) and is the home of the regional blood and marrow transplant (BMT) service.
Ward C9 - Teenage Cancer Trust unit
This area provides specialist care and age-appropriate support to young people aged 13-24 years, who have been diagnosed with cancer. Within the ward there are both inpatient beds and a day unit that offers treatments for cancer that do not require an inpatient stay.
E10 - Apheresis
The apheresis team undertakes the collection of blood stem cells as part of bone marrow transplant treatment and also provides therapies that exchange, remove or collect certain components within blood across a range of differing specialties at CUH.
Ward U3
This ward provides care for haematology and haematological oncology patients undergoing investigations and treatment of disorders affecting the blood or bone marrow. Ward U3 is located on Level 3 of the U block, which is a separate building to the main Addenbrooke’s Hospital. The building can be accessed from Keith Day Road and is on the opposite side of the road to the Cambridge Clinical Research Centre (CCRC).
Ward A5
The Cancer Directorate has two beds on ward A5, which is also part of neuro-sciences department. Primarily these beds are dedicated to the delivery of radioactive iodine therapy. Ward A5 is located on Level 4 of the A block at Addenbrooke’s hospital, which is between the main Outpatients Centre and the main reception.
You will only be admitted to hospital if the nature of your cancer or your treatment makes it impossible for you to remain at home.
CUH Cancer Support Service: Information Team

The Cancer Support Service provides support to anyone affected by cancer, including families, carers, friends and work colleagues, by offering information and signposting to services and organisations that can help with financial, emotional and practical support.
Our Cancer Support Advisors work with people affected by cancer on the wards, in outpatient clinics and in the Information Pod in Oncology and Haematology Outpatients, which acts as a base for the team.
The team has resources in various formats on a wide range of cancer related issues including:
- Treatment side effects
- Emotional impact of cancer
- Diet and nutrition, fatigue, hair loss, managing cancer in the workplace and coping with the financial cost of cancer
- Blue badge information
- Financial support referrals
- Information and signposting regarding hair loss and skin care during your cancer treatment
- Contact details for local support groups suitable for patients, carers and family members
- Signposting to ‘HOPE’ courses (self-management courses)
- Electronic Holistic Needs Assessment (e-HNA) to help identify your main concerns regarding your treatment and life with a cancer diagnosis
Get in touch
The CUH Cancer Support Service is based in the Oncology and Haematology Outpatients Department.
Opening hours: Monday – Friday, 08:00 – 16:00
Anybody can drop in, no appointment necessary.
Tel: 01223 274801
Email CUH Cancer Support Service
CUH Cancer Support Service: Cancer Navigators


Cancer navigators are part of the Cancer Support Service. Their role is to assist and signpost patients with any non-clinical questions they may have as part of their cancer treatment. As the name suggests, they will help you navigate your pathway.
We recognise that a diagnosis of any form of cancer can impact many aspects of your life, but cancer navigators can help to identify what is most important to you and help ensure you and your family receive the most appropriate support.
Navigator help can include, but is not limited to:
- Offering of eHNA (Holistic Needs Assessment), which is a short questionnaire that helps focus on what is important to you. It mainly concentrates on non-clinical concerns you may have at different stages of your pathway
- Information on how to manage practical concerns for example, diet, fatigue and exercise
- Signposting to support groups
- Referrals for emotional support
- Referrals for financial support to check benefits and Macmillan grant eligibility
This list is not exhaustive and navigators can help with other information and support needs. They are able see you face-to-face on site, in clinic or can visit you at your bedside. They can discuss your needs over the telephone or can facilitate an “Attend Anywhere” online appointment. They will be visible on the ward and will look forward to meeting you.

Electronic Holistic Needs Assessment (eHNA)
An eHNA is a tool that allows patients to identify all the concerns they have surrounding their diagnosis and their treatment, so that every patient can receive the correct support at the most appropriate time.
If you are interested in completing an eHNA, or would like more information, please speak to your Clinical Nurse Specialist, Cancer Navigator or one of the Cancer Support Team members.
Additional information about the Holistic Needs Assessment (HNA) is available in the Macmillan booklet, which can be downloaded to your phone by scanning the QR code below:

Your Clinical Nurse Specialist (CNS)
Your clinical specialist nurse’s name is:
Working hours:
Direct telephone line:
Your clinical nurse specialist is an experienced nurse who works with the other members of the team to provide high quality medical and supportive care for you and your family.
The clinical nurse specialist will make every effort to be present at your first consultation to clarify any information and discuss matters important to you. Unfortunately, though, this is not always possible. If they are unable to be there, you will be given a contact telephone number for the specialist nurse so you are able to contact them should you have any worries or need further information when at home. You may have to leave a message, but they, or another member of the specialist team will get back to you as soon as possible.
The clinical nurse specialist will be on hand to co-ordinate any treatment and investigations throughout your treatment and follow-up. Their responsibilities include:
- providing information and support; particularly around side effects and treatment
- ward visits during in-patient stays
- review during chemotherapy treatment
- being present in outpatient clinics (either at nurse-led clinics or reviewing you alongside the medical staff)
- organising and co-ordinating all aspects of your treatment and follow-up
- a point of contact for you and your family
There is usually only one clinical nurse specialist per cancer site and each individual clinical nurse specialist has their own timetable when they may be in clinic, in meetings or elsewhere in the hospital. The nurse is not office-based, so the phone will normally go to voicemail and ask you to leave a message. Your message may not necessarily be answered on the same day but will be answered as soon as possible. Remember, you can also contact your Navigator or the Cancer Support Advisors if your query isn’t clinical.
In emergencies, you should ring the emergency number, not your specialist nurse, so you can talk to someone and obtain immediate advice. This is a 24-hour service. Always carry your emergency contact card with you and put the number into your mobile phone along with your hospital number. You can also give this emergency contact information to close family members.
Emergencies include:
- You have a temperature of 38 o or above
- You feel shivery or flu like
- You feel generally unwell
24-hour helpline contact numbers
Oncology: 01223 274224
Haematology: 01223 274225
Maggie’s Centre Cambridge

If you, or someone you care about is diagnosed with cancer, Maggie’s can help.
Opening times: Monday to Friday, from 9:00 to 17:00
No referral or pre-booked appointment is necessary, just come in.
All Maggie’s support is free.
The centre is a warm and welcoming place on hospital grounds, where you can meet people who are experiencing the same things as you. At Maggie’s, you will find support groups specific to your needs and get advice and information from Maggie’s professional staff. Coming to Maggie’s can help you make positive changes to your lifestyle. The psychological and emotional support offered has been shown to significantly reduce anxiety and depression, and includes:
- Cancer and treatment information
- Cancer-specific support groups
- Help with understanding and claiming benefits
- Exercise and nutrition groups
- Relaxation and stress management
- Support for family and friends
- Bereavement support
Getting to Maggie’s Centre
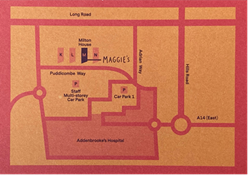
Maggie’s is part of the complex of new flats on Puddicombe Way within Addenbrooke’s site.
There is a free courtesy bus available to use if necessary - please ask at any reception desk for instructions.
Location:
Addenbrooke's Hospital
21 Milton House
Puddicombe Way
Cambridge
CB2 0AD
Getting to the centre by car
You can get to the main building via Addenbrooke's Road entrance, Francis Crick Avenue. Take the first exit on the roundabout at Robinson Way and then take the first right onto Puddicombe Way. Maggie's Cambridge is in the third block of staff residences.

Rehabilitation and Exercise during Addenbrooke’s Cancer Treatment (REACT)
The Rehabilitation and Exercise during Addenbrooke’s Cancer Treatment (REACT) programme is helping people with cancer to stay active following diagnosis and throughout their treatment. REACT provides specialist rehabilitation and therapy to those experiencing musculoskeletal consequences of cancer treatment, and also offers safe exercise opportunities for patients during their treatment at CUH. The programme has enabled rehabilitation to be integrated into cancer treatments across the hospital.
National and international evidence and guidance support the inclusion of physical activity and exercise during cancer treatment and recovery to significantly help, improve or maintain physical function and psychological wellbeing during and after cancer treatment.
Benefits include:
- Reduction in treatment-related side-effects (fatigue, nausea, pain, depression, anxiety)
- Aid overall recovery from surgery and other treatments
- Improve fitness, strength, flexibility and function
- Reduction in the risk of developing other long-term health conditions,
- Improvements in quality of life
- Potential to improve survival
(Stout et al,2021 and Campbell et al, 2019)
The REACT programme is available to patients with all tumour types, throughout their treatment – from diagnosis, through treatment and even for those living with an incurable disease. The programme includes individual therapy assessment and treatment, exercise assessment/exercise counselling, in-person group cardiovascular circuit-style classes (including ‘prehab’) and online education sessions for breast cancer, prostate cancer, colorectal cancer, gynaecological cancer, sarcoma and brain tumours. Introductory sessions to pilates, tai chi, yoga and pelvic floor muscle training are also offered throughout the year.

Please contact:
Clinical Specialist Physiotherapist in Oncology Rehabilitation and Exercise and REACT Lead: Nicola Day
Tel: 01223 349294 (Voicemail Only)
Patient Transport Service
Who can use hospital transport?
Patients are normally expected to make their own way to and from hospital for non-emergency tests and treatments.
However, this may not be possible if you have a medical condition that prevents you from travelling on public transport or in taxis, including taxis with wheelchair access. Where necessary, hospital transport will be provided for both inpatient stays and outpatient appointments.
What are the criteria for hospital transport?
There are clear and consistent national criteria stating which patients can get hospital transport based on medical needs. These criteria apply to both outpatient appointments and discharges from an inpatient stay.
Examples of medical need may include:
- Patients who require a stretcher to travel lying down
- Patients who require oxygen or other medical gases during the journey
- Patients being transferred between hospitals
- Patients who require monitoring during a journey
- Patients whose health would be damaged if they used any other form of transport
- Some patients who use a wheelchair and do not have a wheelchair adapted vehicle
Who decides if you are eligible?
Hospital transport can be arranged by telephoning the EMED Group help desk on 0300 777 5555. Your GP, outpatient clinic or ward will be able to provide contact details if you are outside of the Cambridgeshire and Peterborough area.
A patient’s eligibility for transport is considered each time it is requested, because your medical condition and transport needs can change.
Who provides the hospital transport?
Cambridgeshire and Peterborough - EMED Group is the provider for non-emergency patient transport in Cambridgeshire and Peterborough.
If you are outside this area, please contact your GP, the clinic you are attending or local Integrated Care System (ICS) to find your local provider.
Your transport provider handles transport bookings, queries and any problems with:
- Planned transport
- Late arrivals for planned transport
- Changes in patient appointment times
For outpatients
- If you are unable to attend your appointment or have arranged to make your own way to and from the hospital, please call 0300 777 5555 (for Cambridgeshire and Peterborough area) or your local provider, to cancel your transport.
- Please allow at least 24 hours’ notice to arrange or cancel transport.
- Please ensure you are ready to be collected up to two hours before your appointment.
- Transport may sometimes be late due to unavoidable delays, but every effort will be made to get you to your appointment on time.
- Please bring these with you:
- appointment letter
- any medication and its packaging
- hearing aid and glasses
- key to your home
- Please be aware you may need to share hospital transport with other patients, and therefore have to wait until those patients are also ready to go home.
- Please let outpatient clinic staff know that you are using hospital transport so they can ensure your appointment is kept to time and that you are ready for your return journey home.
For inpatients being discharged
- It is important that you are ready when your transport arrives on the ward.
- Every effort will be made to collect you from the ward promptly, however there are times when transport is unavoidably delayed.
- Please be aware you may need to share hospital transport with other patients, and therefore you may have to wait until those patients are also ready to go home.
Other community transport options in Cambridgeshire
Contact Cambridgeshire Community Transport (opens in a new tab) for further information on any of the following community options in Cambridgeshire:
Community transport schemes in Cambridgeshire
Community transport provides journeys for people who have difficulty using conventional public transport. The majority of the community transport schemes are restricted to individuals meeting the following criteria:
- You do not have access to public transport and do not have access to your own car.
- You experience difficulty using public transport, for example because of a disability or age.
- You are socially or rurally isolated from accessing basic public services and facilities (such as healthcare).
“Taxicard” scheme leaflets
“Taxicard” schemes provide assistance towards the cost of taxi journeys for people who have difficulties getting or using public transport. Please visit the “Taxicard” pages on the Cambridge transport website (opens in a new tab) and select your local area for details.
Further information, concerns or complaints
Please contact the EMED bookings and enquiries help desk on 0300 777 5555 or whoever made the booking (GP practice, call centre, outpatient clinic or hospital ward responsible for the patient’s care), or the local Patient and Advice Liaison Service (PALS) if you need any further information.
Parking for patients undergoing chemotherapy or radiotherapy
Car Parks 1 and 2
Cancer patients receiving chemotherapy or radiotherapy can park in the disabled bays on any level in Car Parks 1 and 2, as they are also designated for cancer patients receiving treatment.
If you are asked for evidence, please present your appointment details.
If you have any further questions, please speak to the staff at the customer service desks which are found on the ground level in both car parks.
Other disabled bays
Other disabled parking bays around the Cambridge Biomedical Campus are only available to blue badge holders.
Car park payments
You can take your car park ticket to Oncology Outpatients or Radiotherapy reception to receive a daily or weekly stamp.
The daily stamp enables you to be charged a discounted daily rate.
The weekly stamp enables you to pay the discounted daily rate for a weekly ticket in case you need to return within one week.
Take the stamped car park ticket to the customer service desks in Car Parks 1 or 2 for processing.
If you have any questions, please ask at Oncology Outpatients or Radiotherapy reception.
If you have a “Blue Badge”, parking is free in both car parks. Take your car park ticket to clinic or outpatient’s reception to get it stamped. When you leave, take your ticket and “Blue Badge” to the park customer service desk for authorisation.
Telephone and video appointments
Since the start of the COVID-19 pandemic, CUH has had to change the way new and follow-up appointments are undertaken. Whilst some will be in person, we also undertake telephone and video consultations. This section provides information about outpatient appointments conducted by telephone and online. A dedicated time slot on a certain day will be allocated to you, but rather than the appointment taking place at the hospital, it will be carried out over the telephone or online.
Why has a telephone/video clinic appointment been suggested to you?
Patients often need to travel long distances to attend specialist clinics. The telephone/video clinic focuses on discussion (about progress, medication changes and management planning) rather than a physical examination. Telephone and video clinics are intended to offer you a more convenient appointment during which health issues can be discussed. As you do not have to come to the hospital, this will save you time and travel.
How does a telephone clinic work?
As with any clinic appointment, you will be sent your clinic letter with date and time in the post and/or via MyChart. During your allocated time, you will be asked to remain close to your telephone and ensure it is not in use. The phone number you will be rung on is entirely your choice, however it is recommended that you use a number which is in a location where you feel comfortable and where confidentiality can be maintained, as the content of discussions may include personal information.
How does a video clinic work?
You will be sent your clinic date and time in the post and/or via MyChart. The link to your video call will be sent to you via email, 15 minutes before the start time of your appointment, or you will be able to access your appointment via MyChart in the ‘Visit details’ page. On MyChart, you will need to click the 'Join video appointment' button, up to 15 minutes before your appointment. The button will be greyed out if you try to join earlier.
When joining the Video Call, the link from the email or the button in MyChart will open Microsoft Teams in a web browser. You will be required to enter your name and allow Microsoft Teams to access your microphone and camera. You will then be placed in a virtual waiting room.
The clinic will see you have arrived, and your doctor will join when ready. You will need to ensure your microphone and camera are both switched on in Microsoft Teams (buttons are in the top right of the screen) and that you do not use the ‘Chat’ feature in Teams during your appointment. You will also need to ensure you are in a quiet and private place to have your appointment, as the content of discussions may include personal information
What if you prefer to come to a hospital-based clinic?
The choice to attend a hospital-based clinic is entirely yours. The telephone or video clinic appointment is offered to you as an alternative to a face-to-face clinic appointment. If you prefer to attend a hospital-based clinic instead of your arranged telephone or video appointment, please contact the relevant department on the number provided within your clinic letter. Please be mindful of the waiting times for the face-to-face clinic appointments, as these require booking in advance.
You are welcome to attend hospital outpatient clinics as before at any time.
Will you always be followed up in this manner?
Not necessarily. If you have no new symptoms or concerns that need action, then telephone or video clinics are ideal. If we need to see you to undertake a physical examination, tests or investigations, we will ask you to come to the clinic.
What if you are not going to be available at the date and time of the telephone or video appointment?
If you are going to be unavailable for a scheduled telephone or video appointment, it is essential that you contact the department to arrange a different appointment time that is convenient to you, and also to enable us to offer your appointment slot to another patient.
What happens if you don’t answer the telephone or attend video consultation at the time of your appointment?
If you do not answer the telephone or attend video consultation within the first few minutes of your appointment time, it will be recorded that you did not attend (DNA) the consultation.
Making the most of your telephone/video clinic appointment
The Addenbrooke’s Cancer Patient Partnership Group (CPPG) has listed some tips below on how to make the most of your telephone or video clinic appointment. Not all these tips may apply to you.
Before the call
1. Write down your symptoms and concerns to help you organise your thoughts more clearly and to decide what’s relevant and most important. It may be helpful to review any previous letters, results, documents, etc.
2. Write down any questions you may have.
3. Perform any agreed checks or tests that the clinician has requested or might expect well before the consultation so you are aware of any new issues and can discuss or ask about them, for example a self-examination. If you need to have blood tests done, you may be able to have them done at your GP surgery but check with your GP and treating team well in advance (at least a week).
4. You may wish to invite a family member to join the meeting to take notes and ask questions that may not occur to you. Remind them again before the meeting so they are ready.
5. Have the following items to hand:
a. Pen and paper
b. Medications you are taking
c. Previous notes or letters
d. Glass of water and tissues
e. Reading glasses if you need them
f. Hearing aids if you need them
6. Prepare to take the call at the appointed time but be aware that the call may be slightly early or delayed.
7. Choose a quiet, well-lit and, where possible, private location. If possible, consider proximity away from noisier areas of the property/ your home (including bathrooms).
8. Limit distractions, ensure that you are free from interruptions from children and pets; request household members to ‘do not disturb’. Perhaps place a sign outside the door. If not using it, turn your mobile phone to vibrate / silent.
9. Where possible designate someone else to deal with outside distractions, for example the doorbell.
10. Set a reminder alarm for half hour before the meeting to remind you to set up and be ready at least five minutes prior to the appointment start. In the case of a video call this provides an opportunity to run through checks: clear image, lighting, appropriate volume, etc.
11. You may wish to put the call on speaker phone so that a family member/carer can also listen in – check that you know how to do this.
12. If you prefer a video call, you can ask if this is currently possible. Contact your treating team by phoning the number on your appointment slip or if you use MyChart, contact the number within Your Appointment Details.
13. For a video call, consider your attire and what you may possibly need to remove/adjust to show the clinician any relevant parts of your body. You may need an additional lamp for illuminating required close-up views.
14. If you have been offered a video appointment, you can read more about how to access it here: Video appointments
During the call
1. The call will be shown as “No Caller ID” with the number withheld. If you cannot pick up or get disconnected, wait for the clinician to call you back. If you have not heard within two hours, contact your treating team by phoning the number on your appointment slip or if you use MyChart, contact the number within Your Appointment Details.
2. If the connection is not clear, insist on trying to re-connect or use a different phone.
3. If you want to record the call, check that this is okay with the clinician.
4. Let the clinician know if you have the phone on speaker and who is with you.
5. Share your symptoms or main concerns at the beginning of the call. It is important to be clear and specific since the clinician cannot see you to get an impression. Before the call you could ask if you can share the information via MyChart or email.
6. Take notes or ask a family member to do this for you.
7. Don’t hesitate to check your understanding by repeating back what you heard or by asking questions.
8. If blood or scan results are not available for the call, ask when they will be.
9. Ask for a summary letter to be written directly to you with a copy to your GP, including any biopsy and scan results.
10. Make sure you know and record the outcomes and have contact details for any queries that may crop up. For example, if you are being sent an exercise sheet or other literature it may not be totally self-explanatory and you may need to clarify the information.
11. Consider using BRAN (see below) to guide your discussion. What are the:
Benefits?
Risks?
Alternatives?
(Do) Nothing?
After the call
- When you receive your summary letter check that the contents match what you agreed. If not, contact your treating team.
MyChart
MyChart is the electronic patient portal at CUH which enables patients to securely access parts of their health record held within the hospitals’ Epic electronic patient record system. It can be accessed via a desktop or smartphone.
Why use MyChart?
If you have not already done so, we would encourage you to sign up for MyChart as our hospital information will be available to you electronically in MyChart including:
- upcoming appointments/past appointment details
- current problems/conditions
- clinical correspondence
- vital signs (weight, height, blood pressure, temperature, pulse, respiration)
- test results
- medications
- known allergies
- demographic information (name, date of birth, address, GP details)
- medical and family history
- implant activity (if applicable)
There is also functionality within MyChart that enables you to:
- message your care team (if available within the clinical specialty caring for you)
- download your recent visit records
- securely share your MyChart information electronically with clinicians outside of Addenbrooke’s hospital and the Rosie, for example your GP, community care staff, clinicians at other hospitals caring for you (via ‘Share Everywhere’ within MyChart)
MyChart is designed to improve communication between you and your clinical teams and enable you to be more involved and informed about your care by having access to your information. You will receive an email alerting you to any new message or information in MyChart.
Interested in using MyChart?
To sign-up to MyChart you can either:
- Complete the online registration (opens in a new tab) or
- speak with a clinic receptionist or your clinical team about MyChart sign-up during your next appointment
Once you have signed-up, you will be able to access your hospital information via MyChart from your smartphone or tablet device (Apple or Android) or from a computer or laptop. MyChart is compatible with screen readers.
Accessing MyChart
- Website - log in to your MyChart (opens in a new tab)
- Smartphone - you can download the MyChart app on smartphone or tablet devices (Apple or Android) then choose ‘Cambridge University Hospitals’ when prompted to select a hospital within the app.
Questions about MyChart?
If you have any questions about using MyChart please complete the ‘Contact Us’ form (opens in a new tab) available on the MyChart website and app.

Cancer Research UK (CRUK)
Cancer Research UK (CRUK) funds life-saving research in Cambridge, united under the CRUK Cambridge Centre. The Centre brings together over 1,200 world-leading scientists, clinicians, nurses, healthcare professionals and industry partners from across the Cambridge area to tackle cancer from every angle. As a partnership between Cancer Research UK, the University of Cambridge and Addenbrooke’s Hospital, CRUK research is focused on detecting cancer at its earliest stage and treating it more precisely to improve patient outcomes.
CRUK also funds individual researchers and labs across the region, and institutes at the University of Cambridge, including the Welcome/CRUK Gurdon Institute and CRUK Cambridge Institute. The CRUK Cambridge Institute is located on the Cambridge Biomedical Campus, just around the corner from Addenbrooke’s Hospital, and houses over 300 cancer scientists researching the prevention, diagnosis and treatment of cancer.
Find out about the CRUK research
You can find out how the research is making a difference to patients by visiting the CRUK websit (opens in a new tab), by following CRUK on Twitter (@CRUKCamCentre) or by listening to the CRUK podcast (opens in a new tab).
In the podcast, the scientists, clinicians, health professionals and patients discuss everything about CRUK work from how the latest advances in imaging and genomics are used to personalise treatment, to keeping fit with pancreatic cancer. You can also submit your suggestions for future episodes at Submit suggestion (opens in a new tab).

How to get involved
CRUK involves patients and the public at all stages of their work from advising strategy, to shaping the research and clinical trial proposals, to participating in clinical trials and research studies. CRUK has patient and public involvement (PPIE) groups focused on different areas of research, including breast cancer, ovarian cancer, pancreatic cancer, clinical trials and radiotherapy. If you would like to find out more about the PPIE groups and join CRUK in shaping future research, please email the engagment team.
Radiotherapy timeline

Please check out the “Timeline of Radiotherapy” display next to the Radiotherapy reception area. The display explains what radiotherapy is, highlights the machines involved and how they work, and, most importantly, it celebrates how patient and public voices have been essential in the development of radiotherapy services for many decades. You can also watch the CRUK Virtual Timeline of Radiotherapy video (opens in a new tab) .
If you've been diagnosed with cancer, or know someone who has, the CRUK provides practical information on everything from symptoms and screening, to coping after treatment. Please visit the CRUK website (opens in a new tab).
Patient Advice and Liaison Service (PALS)
If you, a family member, carer, or friend have any questions, would like more information, or have a concern about your care or treatment, please speak directly with the person providing the care or treatment in the first instance. This could be a nurse or matron, a doctor, or another health professional. They will try to resolve your concerns right away.
If you have tried speaking to a member of staff looking after you and you are still concerned, you should ask to speak to the person in charge. If for any reason you feel unable to speak with the person in charge or talking to them has not helped, please contact the Patient Advice and Liaison Service (PALS). The PALS team will listen to you and work with you to achieve a satisfactory resolution whether you are requesting information, providing feedback, raising a concern, or needing information about making a complaint.
Patient Advice and Liaison Service can:
- Advise and support you and your family, and act on your behalf
- Listen to your suggestions for improving our service for patients and visitors
- Help resolve your concerns if you are unhappy with any aspect of your care
- Pass on your compliments to staff if you are pleased with the way they cared for you
Contacting Patient Advice and Liaison Service

Tel: 01223 216756
Opening times: 10 am to 3 pm, Monday to Friday
Inpatients: you can telephone free from your Hospedia telephone, please call *801.
The team can also visit you on the ward to discuss your concerns.
You can also drop-in to PALS, who are located near the main Addenbrooke's Hospital reception, Monday to Friday, from 1 am to 3 pm. (closed weekends and Bank Holidays).
Or fill in the PALS online form
- The PALS team will acknowledge your contact as quickly as possible and aim to answer questions and resolve any issues within ten working days, however this may take longer in some circumstances.
- A friend or relative can contact PALS on your behalf, but your permission must be given before the team discusses your personal circumstances with anyone else.
- It is helpful to provide your hospital number or NHS number when you contact PALS.
If the PALS team cannot resolve your concerns, or if you would like to register your issues more formally, you may wish to raise a complaint.
Carers
Caring often begins at home but many people never think of themselves as carers: they are partners, spouses, children, relatives and friends. Carers are people who care for a family member, a friend or another person in need of assistance or support with daily living. They include those caring for the frail aged, people living with long-term medical conditions, people with a mental illness, people with a disability and those receiving palliative care.
Carers’ passport
Some carers wish to continue their caring role, for example assist with personal care, whilst the patient is in hospital. CUH will always aim to support this, but carers should not feel obliged to continue with their caring role. Carers’ passports are yellow ID cards worn by a carer so that they can be easily identified by staff. The passports are issued to carers after discussion and agreement with the patient, carer and staff about the caring duties that the carer wishes to continue.
When you are admitted to a ward or must attend the Emergency Department, ask the nursing staff about a carers’ passport, if you would find this helpful. The passport may enable a carer to have access to the ward outside normal visiting times in order to enable caring duties to continue. If the patient is attending the Emergency Department, this can help prompt a conversation with staff regarding the need for a carer to stay with the patient.
If you are attending an outpatient appointment and you would like to be accompanied by your carer, perhaps to assist with communication or provide mental health support, the person that requires a carer’s passport can call the Accessibility Team on 01223 256998 or email the accessibility team. The Accessibility Team, based at outpatient main reception, have a supply of carer’s passport agreements and badges as does the reception team in Clinic 12.
Carer’s Checklist
- Tell the staff looking after the patient that you are their carer
- Find out about a Carer’s Passport - ask the staff looking after the person you care for
- Ask to be involved in conversations about the patient’s care and discharge from hospital,
- Check transport arrangements for getting the person you care for to and from hospital,
- If you live some distance away, look into accommodation options.
- Have you registered a What IF? Plan with Caring together (opens in a new tab)?
- Are you registered with your local carers’ support organisation?
- If you have your own health appointment and think you might not be able to attend because of your caring responsibilities, contact Caring Together (opens in a new tab) to see if they can help.
Car parking for carers
CUH offers discounted car parking rates for people who are regularly visiting patients in hospital. Full details can be found on entry to the car parks, at the pay stations and the customer service desks situated in the car parks, or on the CUH car parking pages of the hospital website.
Support for Carers in Cambridgeshire and Peterborough

Care Network
Tel: 0195 4211919
Care network website (opens in a new tab)
Supports all adults to live well, independently and keep in touch with their community. Community Navigators can help with finding local support and things to enjoy.

Caring Together
Tel: 0345 2410954
Caring together website (opens in a new tab)
Supports carers aged over 18 caring for people of any age with any illness or disability. Offers groups where carers can meet other carers for support.

Centre 33
Tel: 0333 4141809
Centre 33 website (opens in a new tab)
Supports young people aged 18 and under who look after a family member. Supports with moving to secondary school, college or university. Undertakes assessments to identify needs and reduce impact of caring.

Making Space
Tel: 01480 211006
Making space website (opens in a new tab)
Supports carers who look after someone living with a mental health condition aged between 18 and 65 years old. Offers carer support groups and coffee mornings held across Cambridgeshire and Peterborough.

Healthwatch
Tel: 0330 355 1285
Healthwatch Cambridgeshire website (opens in a new tab)
Healthwatch Peterborough website (opens in a new tab)
Speaks up for people who use NHS health and social care services.
To find further information about cancer support services in your local area wherever you are in the UK, you can use the Cancer Care Map (opens in a new tab).
For information about how CUH supports carers, or if you have any suggestions or concerns about support provided for carers, contact the Patient Advice and Liaison Service on 01223 216756 or email CUH PALS.
Additional resources
There is a wide range of literature available depending on your personal needs. Listed below are some of the more frequently used titles, all of which can be accessed via the Cancer Support Information Service, or through the Macmillan website. They can also be downloaded to your phone by scanning the QR code.
Macmillan Cancer Guide (opens in a new tab)
This is a guide about cancer treatment and care. It explains the different stages people go through when they have cancer, the roles of various cancer care professionals and how to get additional support and information.
Being diagnosed with cancer can be a huge shock. You may be feeling lots of different emotions. But it does not mean you have to give up hope. Many people are now treated successfully or able to live with cancer for many years. There are lots of people and services that can support you.

Macmillan: Healthy Eating and Cancer (opens in a new tab)
This booklet has been written for people living with or after cancer, who want to know more about a healthy diet. It explains why diet is important and has tips on how to eat well and maintain a healthy body weight. It aims to help you think about what changes you may want to make, and to help you put them into practice.
Many people want to make positive changes to their lives when they have been diagnosed with cancer. Taking steps to live a healthier lifestyle is often a major part of these changes.

Macmillan: Help With the Cost of Cancer (opens in a new tab)
This booklet explains the types of financial help you could get and how to claim this support. It also tells you who to contact for further help, including the welfare rights advisers.
This booklet also includes quotes from people affected by cancer who have shared their experiences of managing money.
A cancer diagnosis can change your financial situation. It may mean you need to stop working or work less. It can also mean spending more money on things like hospital parking. But depending on your situation, you may be able to get benefits or other financial support.

Macmillan: Physical Activity and Cancer (opens in a new tab)
The booklet explains what physical activity is, its benefits and
how to be safe when exercising. It includes information
about the types of activities you can do and how to get started. There is also information for carers, family members and friends.
Physical activity is any type of exercise or movement that uses your muscles. This includes everyday activities such as walking, housework and gardening. Any type of activity will help maintain or improve your fitness, health and well-being.

Macmillan: Life after Cancer Treatment (opens in a new tab)
The booklet is about coping after cancer treatment finishes,
including managing side effects, follow-up care, and making healthy lifestyle changes. It is for people who are preparing for life after cancer treatment.
This booklet can help you deal with some of the questions or feelings you may have.

Macmillan: How are you feeling? The emotional effects of cancer (opens in a new tab)
Having cancer affects all areas of your life, including the way you feel. This booklet is about the emotions that many people with cancer have. This may be after diagnosis, during treatment or after treatment has ended.
This booklet can help you in dealing with some of the feelings that you may have.

Psychological/Emotional Support
There are a number of support options for people experiencing emotional or psychological distress as a result of a cancer diagnosis. For specific advice, please contact the Cancer Support Information Service directly.
This is only a very small sample of what is available, so if you would like information on a particular topic, or if you have any questions about cancer, please email the Cancer Support Information Service directly or call 01223 274801. The team will be able to help you find what you need.
Macmillan also provides a wide range of resources for people who do not have English as a first language, or for people with a range of sensory and cognitive impairments. These can also be accessed through the Cancer Support Information Service near Oncology reception.
Additional information
Food Court and Concourse
The Food Court and Concourse at CUH includes eating and drinking areas such as Costa, Starbucks, Marks & Spencer and Burger King. These areas are located on level 2 of the main hospital (circled on the map of the Cambridge Biomedical Campus).
The easiest way to access the Food Court and Concourse is via the main hospital entrance. Please enter the main hospital entrance and turn right. Go through a set of double doors and continue straight; the Food Court is located on the right. The Food Court is approximately 37m from the main hospital entrance. Wayfinding signage is provided. Opening times may vary.
Please be aware: The flooring in corridors of the Food Court and Concourse is shiny and could cause issues with glare or look slippery to some people.
Map of the Cambridge Biomedical Campus
Prescription charge exemption form (FP92A)
To apply for a medical exemption certificate, which entitles you to free NHS prescriptions, you will be required to fill the “Application for prescription charge exemption (medical)” form. Ask your GP or collect the form from the Cancer Support Information Service if you need one. Your GP or the medical team looking after you at CUH will sign the form to confirm that your statement is correct.
CUH and Net Zero
As a department we want to do our bit towards the NHS target of reaching Net Zero by 2040. If you are receiving treatment with us, you can help us reach our goal of becoming environmentally sustainable by doing the following things:
- When you are dealing with clinical teams/support services, if you are happy to receive information in electronic rather than paper format, can you let us know?
- Can you bring a reusable water bottle when you come for your treatment?
- Can you let your doctor know if you have lots of extra of your medications at home already, so we don’t give you anymore?
- Could you take plastic home to recycle rather than putting in a hospital bin, and take your empty medication blister packs to be recycled at a local recycling scheme e.g. Superdrug?
- If you’re feeling well enough, could you have your appointment by telephone/video follow ups, or attend the hospital by bus or bike?
Thank you
References:
- Stout, N.L, Santa-Mina, D., Lyons, K.D., Robb, K & Silver, J.K. (2021). A Systematic Review of Rehabilitation and Exercise Recommendation in Oncology Guidelines. Canadian Cancer Journal Clinics. Volume 71 pp. 149-175.
- Campbell, K.L, Winters-Stone, K, Wiskemann, J, May, A. et al (2019) Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Medicine & Science in Sports & Exercise: November 2019, Volume 51, Issue 11, p.2375-2390. Available at: Guidelines for Cancer Survivors (opens in a new tab)
Privacy and dignity
Same sex bays and bathrooms are offered in all wards except critical care and theatre recovery areas where the use of high-tech equipment and/or specialist one to one care is required.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

