Pancreatic cancer occurs when abnormal cells in the pancreas start to divide and grow in an uncontrolled way, forming a growth (tumour).
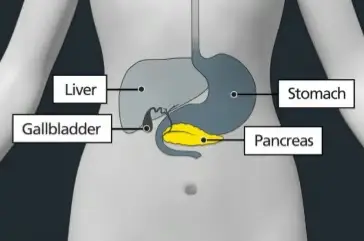
The pancreas is a long gland located in the upper abdomen, behind the stomach. It is part of the digestive system. The pancreas is responsible for production of digestive juices, called enzymes, and production of hormones including insulin.
Often pancreatic cancer may not cause any symptoms, or they might be hard to spot.
Symptoms of pancreatic cancer can include:
- jaundice - the whites of the eyes or the skin turn yellow
- loss of appetite or losing weight without trying to
- tummy or back pain
- feeling or being sick
- changes in your poo
Pancreatic cancer is broadly classified into two main types:
- exocrine tumours
- neuroendocrine tumors
The most common type of pancreatic cancer is pancreatic ductal adenocarcinoma (PDAC), which is an exocrine tumour that originates in the lining of the pancreatic ducts.
Other, less common exocrine tumour types include:
- acinar cell carcinoma
- cystic tumor
- intraductal papillary mucinous neoplasm (IPMN)
Neuroendocrine tumors, also known as pancreatic neuroendocrine tumors (pNETs), are less common and originate in the hormone-producing cells of the pancreas.
Treatment for pancreatic cancer at CUH
The treatment you have depends on several factors, which include:
- the type and size of the cancer
- where the cancer is located in the pancreas
- if the cancer has spread
- your general health
A team of specialists at CUH will meet to discuss your condition and to make a recommendation about the best possible treatment for you.
You, along with your clinician, will then discuss your treatment recommendations at the clinic appointment and decide on the right treatment plan for you. Your clinician will explain different treatment options and possible side effects.
Pancreatic cancer can be difficult to treat.
The treatment for pancreatic cancer can include:
- surgery
- chemotherapy
- radiotherapy
- symptom control/supportive care
You may be able to have surgery to treat pancreatic cancer. Surgery can remove part or, in some cases, all the pancreas. All or parts of other organs surrounding the pancreas may also need to be removed. Recovery from surgery to treat pancreatic cancer can take a long time.
At times, you may require more than one treatment or a combination of different treatments to give the best chance of long-term cure.
Read more about the different types of treatment on our website.

