Myeloma (sometimes called multiple myeloma – these terms are used interchangeably and refer to the same condition) is a type of blood cancer arising from plasma cells, which affects the bones and different parts of the body.
Plasma cells are a type of white blood cells made in the bone marrow. Bone marrow is a spongy tissue found inside the bones, where blood cells are made.
Plasma cells form part of the immune system, and their role is to make antibodies, also called immunoglobulins. Antibodies circulate in the blood, find and help with removing germs such as viruses, bacteria and fungus and therefore help fight infections.
Myeloma develops when the bone marrow makes plasma cells that do not work properly. These abnormal cancerous plasma cells then make abnormal antibodies, known as paraprotein, which cannot kill germs effectively and have no useful function within the body. These cells multiply and spread within the bone marrow. Most of the medical problems related to myeloma are caused by the build-up of abnormal plasma cells in the bone marrow and the presence of the paraprotein in the body.
Unlike many cancers, myeloma does not exist as a lump or tumour - it can affect multiple areas in the body where the bone marrow is normally active, such as the bones of the spine, skull, pelvis or rib cage.
Myeloma does not always cause symptoms in its early stages, but might be picked up on a routine blood test.
When it however becomes symptomatic, the main signs can include:
- bone pain - often in your back, hips, shoulders or ribs
- fatigue - feeling very tired for no reason
- shortness of breath
- muscle weakness
- headaches
- recurrent infections including ones that may require hospital admission or rarely can be life-threatening
- feeling very thirsty and needing to pee more often than usual
- losing weight without trying
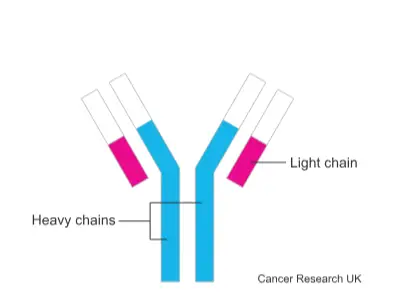
There are different types of myeloma depending on the type of paraprotein and light chains in your blood. Each paraprotein is made up of:
- 2 long protein chains, also called heavy chains
- 2 shorter protein chain, also called light chains
This is important because sometimes myeloma doesn’t make the whole paraprotein. Sometimes it only makes large amounts of the light chain part of the paraprotein. These are called free light chains or Bence Jones proteins.
There are different types of heavy and light chains. These are described below:
- Heavy chain - 5 types: G, A, D, E and M
- Light chain - 2 types: kappa and lambda
Your myeloma will only make one type of paraprotein (abnormal immunoglobulin), either G,A,D,E or M. and your doctor will name your myeloma after one of those abnormal immunoglobulin types and the type of the light chain, either kappa or lambda.
Based on this, your doctor might say that you have, for instance, IgG kappa myeloma.
IgG (immunoglobulin G) is the most common type of myeloma, followed by IgA myeloma. IgM, IgD and IgE are very rare.
After genetic tests, you may also be told that you have a particular genetic subtype of myeloma. This information gives doctors a better idea of how the myeloma might progress.
The sub-types of myeloma can include:
- Light chain myeloma
- Non secretory myeloma (myeloma with very limited or no paraprotein / light chain production)
- Smouldering myeloma (myeloma without symptoms)
Treatment for myeloma at CUH
The treatment you have depends on several factors, which include:
- the specific type of myeloma
- the stage and progression of the disease
- your age and general health
A team of specialists at CUH will meet to discuss your condition and to make a recommendation about the best possible treatment for you.
You, along with your clinician, will then discuss your treatment recommendations at the clinic appointment and decide on the right treatment plan for you. Your clinician will explain different treatment options and possible side effects.
The treatment for myeloma can include:
- chemotherapy
- radiotherapy
- targeted immunotherapy
- steroids
- bone marrow (stem cell) transplant
- CAR-T cell therapy
- bisphosphonates
At times, you may require more than one treatment or a combination of different treatments to limit the cancer and its symptoms and help you live longer.
Myeloma cannot usually be cured, and in a smaller proportion of patients, it might be very hard to treat. Your clinical team will discuss with you what to expect and will help you control the cancer and manage your symptoms.

